
Glaucoma
The Collaborative Initial Glaucoma Treatment Study (CIGTS)
The Collaborative Initial Glaucoma Treatment Study (CIGTS)
Objective: Open-angle glaucoma is a major cause of reduced vision both in the United States and internationally. The Collaborative Initial Glaucoma Treatment Study aimed to determine whether patients with recently diagnosed open-angle glaucoma had better outcomes when initially managed with medications or with immediate filtration surgery.
Design: Randomized, controlled clinical trial of 607 patients from 14 clinical centers.
Patients with newly diagnosed open-angle glaucoma were randomized across age, gender, race and type (primary, pigmentary pseudoexfoliative open-angle glaucoma) to initial medication treatment (n = 307) or initial trabeculectomy (n = 300).
All patients had two visits prior to randomization where intraocular pressure (IOP) was checked six times total, in addition to two visual field (VF) tests, allowing for creation of mean reference values for each patient.
Patients were followed every 6 months for 9 years for VF, IOP and visual acuity testing
Surgical arm: Underwent trabeculectomy with or without 5-fluorouracil within 14 days of randomization. If intervention failed, patients received laser trabeculoplasty, followed by a series of medications and repeat trabeculectomy with antibiotics and medications.
Medication arm: Patients typically were started with a topical beta blocker, followed with an alternative topical medication, then dual topical therapy, triple topical therapy, alternate triple topical therapy and finally an optional additional topical and/or oral medication. If the intervention failed, patients received the following escalating treatments: laser trabeculoplasty, trabeculectomy, medication and finally trabeculectomy with an antifibrotic agent and medication.
Intervention failure: Determined based on progressive VF loss or failure to meet target IOP at two consecutive follow-up visits as determined by patient’s reference IOP from initial baseline visits.
Target IOP = (1- [reference IOP + visual field score] /100) X reference IOP)
Inclusion Criteria:
Primary open-angle, pseudoexfoliative or pigmentary glaucoma in one or both eyes
One of 3 combinations of qualifying IOP, VF changes and optic disc findings:
IOP of 20mmHg or higher with definitive VF loss and optic disc findings compatible with glaucoma
IOP of 20 – 26mmHg with likely VF loss and glaucomatous optic disc damage
IOP of at least 27mmHg with glaucomatous optic disc damage
Visual acuity score of 20/40 in each eye
Age between 25 and 75
Exclusion Criteria:
Cumulative use of glaucoma drops that exceeded 14 days in lifetime
Use of glaucoma eyedrops 3 weeks before baseline visit
Ocular disease other than glaucoma that could alter IOP, visual function, visual field testing, aqueous flow
Proliferative diabetic retinopathy, diabetic macular edema, nonproliferative diabetic retinopathy w/ > 10 microaneurysms
History of ophthalmic laser, refractive, conjunctival or intraocular surgery in either eye
Current or expected use of corticosteroids
Primary Outcome: Sustained progression over a year in visual field loss as represented by a mean deviation decrease in the visual field score by 3dB or more from reference value.
Visual fields assessed using the Humphrey full threshold 24-2 testing strategy
Secondary Outcomes: Health-related quality of life, visual acuity and IOP
Health-related quality of life measured by questionnaire.
Visual acuity measured using test charts at 4m before pupil dilation.
IOP tested using Goldman applanation device before gonioscopy or dilation.
Mean Baseline Characteristics: 607 patients enrolled, 55% male, average IOP 27mmHg, mean deviation of visual field testing -5.5dB, average C:D .7, 1st degree FHx ~33%,
Results:
90% of participants were active at 5-year follow-up, but at 9 years, this was reduced to 27%
Primary outcome:
Visual field scores
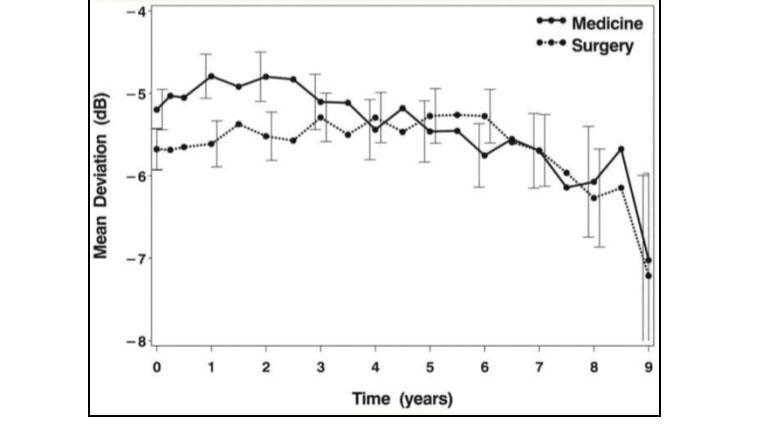
At 8-year follow-up, patients who received surgery initially had worsening mean deviation in visual field from -5.3 to -6.3, while the medically treated group worsened from -5.5 to -6.1 (Figure 1).
25.5% of the medically treated group and 21.3% of the surgically treated group had substantial VF progression (>3dB) at 9 years.
Patients who presented with worse initial VF had less VF loss over time when treated surgically
Worsening visual field scores was also associated with worse baseline VF scores, old age, nonwhite race and diabetes.
Patients with diabetes had reduced VF loss when treated medically rather than surgically (1.89dB loss in the medical group vs 2.65dB loss in the surgical group average from year 2 to year 9).
Secondary Outcomes: Quality of life, visual acuity and IOP
Quality of life:
Only minor differences in quality of life between the two intervention groups at 5-year follow-up.
Patients in the trabeculectomy group reported increased rates of eye irritation and ptosis at 5 years.
Medically treated patients reported increased systemic symptoms such as drowsiness and headache early in treatment, though these symptoms were not reported at the 5-year follow-up.
Visual Acuity
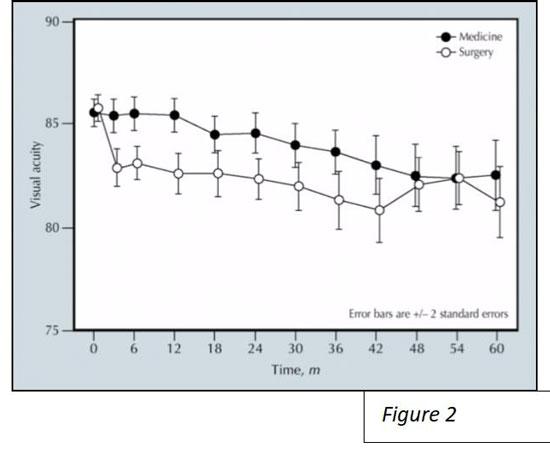
In the first year, patients assigned to trabeculectomy suffered 3-letter loss of vision, while visual acuity was stable in the medically treated group (Figure 2).
At 5-year follow-up, both groups had reduced vision with 3.9% of medically treated patients having > 15 letter loss in visual acuity vs. 7.2% of those surgically treated.
Medically treated patients were less likely to develop cataracts than those treated surgically.
Predictors of vision loss: initial surgical treatment, cataract development, nonwhite race, diabetes and worse baseline vision.
Intraocular Pressure (IOP):
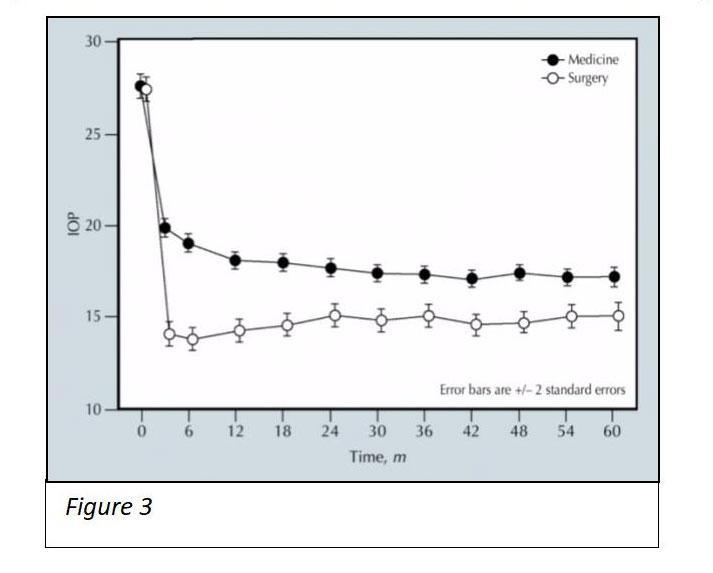
Surgery lowered IOP to 14-15mmHg on average, while medical therapy lowered it to 17-18mmHg from respective baseline at ~27mmHg (Figure 3).
IOP was lower in the surgical intervention group at all points.
In both groups, ~8% of participants failed intervention and needed additional therapy.
Take Home Points:
9-year outcomes show that both surgery and medication interventions are effective at reducing intraocular pressure, with similar results in visual field progression.
Patients who present with moderate to severe VF may benefit from earlier surgery.
Trabeculectomies are not without risks: Patients were more likely to develop cataracts and experienced more local eye symptoms than the medically treated group.