InSight Newsletter
InSight Newsletter Winter 2026
Message from the Chair
Welcome to the Winter 2026 edition of the Department of Ophthalmology InSight Newsletter.
This issue's research spotlight is on George and Martina Krem Associate Professor Ram Sabesan’s recently published study establishing the utility of a new technology developed in his lab, called optoretinography. This precision engineering method has emerged as a tool that can predict the course of degenerative retinal disease earlier than any conventional diagnostic method.

Our Patient Care Spotlight welcomes a new pediatric ophthalmologist and a new optometrist to the faculty: Assistant Professor Jeannette Stallworth, MD and Jeff Dabundo, OD.
Dr. Stallworth completed her pediatric ophthalmology fellowship with us in 2024, and we are delighted to have her back on the team at Seattle Children’s.
Dr. Dabundo will serve in a new role as a triage optometrist at the Eye Institute, providing urgent eye care to patients with new-onset ocular symptoms and appropriately referring them to ophthalmology specialty care, as needed.
In Education, we are proud to announce our new class of fellows for 2026-27, and our class of 2030 residents. We will have seven fellows joining us in July, including new fellowships in neuro-ophthalmology and ocular oncology. Our residency class has expanded to include a sixth position.
Finally, in our philanthropy spotlight, learn more about a transformational gift from Dawn’s Light Foundation to create a purpose-built clinical trials center in the South Lake Union F Building. Opening this summer, the new facility will house up to 10 staff members and optimize patient care, study coordination, and research activities. This enhanced infrastructure will ensure that Ophthalmology’s clinical trials program can continue to pursue cutting-edge discoveries and bring emerging therapies to patients more efficiently.
Russ Van Gelder, MD, PhD,
Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Director, Roger and Angie Karalis Johnson Retina Center
Director, Vision Science Center
Study validates split-second exam of retinal health
UW Ophthalmology researchers have validated an approach to measuring how rod photoreceptors, the cells in our eyes responsible for night vision, respond to light in living eyes. The approach might one day enable earlier detection of serious eye diseases, such as age-related macular degeneration (AMD).
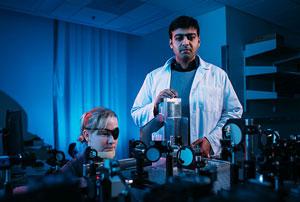
In studying the normal, healthy retinas of humans and rats, the investigators reported seeing consistent cellular-level responses to a prescribed amount of light: The outer segments of the rod photoreceptors shrank immediately and rapidly, then slowly elongated.
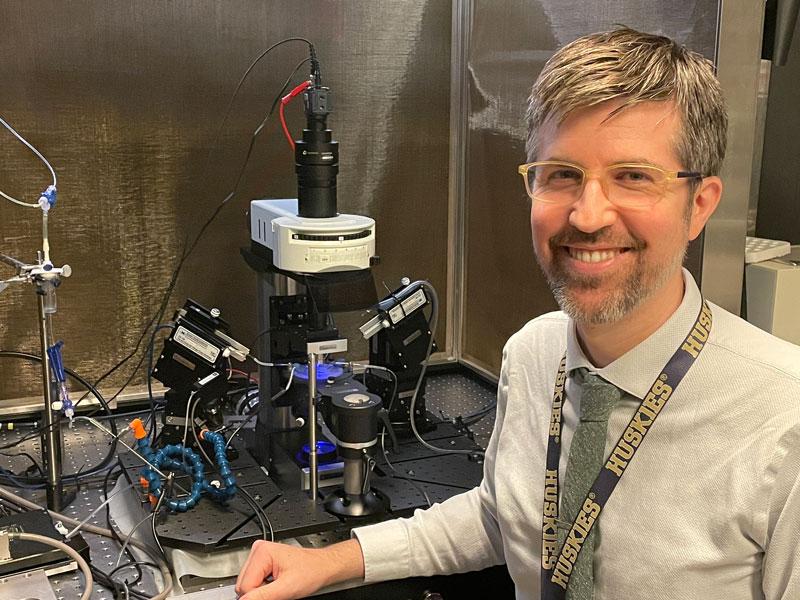
"This is the first time we've been able to see this happen in rod cells in a living eye," explained Ram Sabesan, George and Martina Kren Associate Professor of Ophthalmology at the University of Washington School of Medicine. He was the co-corresponding author of the study, published in the journal Light: Science & Applications.
The findings, he said, reinforce the feasibility of a novel technology called optoretinography. In just a few years, it has emerged as a tool that might predictably display molecular hints of retinal disease earlier than any conventional diagnostic instrument.
“Rod dysfunction is one of the earliest signs of many retinal diseases, including AMD and retinitis pigmentosa,” Sabesan said. “Being able to directly monitor the rods’ response to light gives us a powerful tool for early detection and tracking treatment responses.”
In 2020, he and colleagues published findings about optoretinography’s ability to show similar shrinkage in cone receptors, the specialized cells responsible for color and daytime vision.
Seeing similar action with the smaller rod structures was “like watching the eye’s molecular machinery spring into action in real time, without electrodes, dyes or surgery,” said Tong Ling, assistant professor at Nanyang Technological University, Singapore, and the study’s co-corresponding author. He was also a coauthor of the 2020 findings.
In this study, Ling’s team measured rod cells’ response in rats while Sabesan tested the eyes of three people. Both exams showed minute contractions of rods’ outer segments that occurred within 10 milliseconds of light exposure — a span shorter than a single flap of a hummingbird’s wings.
Optoretinography integrates multiple technologies. One is adaptive optics, used by astronomers to compensate for atmospheric turbulence and generate sharp pictures of stars and other celestial objects. Incorporating adaptive optics into a conventional retinal camera enables the differentiation of rods from cones in the human eye.
Another is interferometry, which splits a beam of light into two paths and recombines them to create patterns of light and dark that allow scientists to precisely measure minute distances and surface irregularities.
As a result, Ling said, ophthalmologists can distinguish and measure cellular structures with “far higher spatial resolution [than conventional diagnostics] while making the detection process completely contactless.”
Sabesan acknowledged that this testing is “in early days and not a readily available diagnostic for clinical use.” He described the optoretinography test setup as “decidedly homemade,” with components covering most of a 4-by-8-foot table.
Its promise, though, is to outperform current diagnostics of retinal function such as electroretinography, which he said lack sensitivity, take significant time and can be onerous for patients.
The next step, Sabesan suggested, would be to study rod photoreceptor function in larger patient cohorts, including people with elevated disease risk and those already diagnosed with age-related macular degeneration, to ascertain early manifestations of the condition.
Beyond mapping rod dysfunction, the findings also hint at personalized, noninvasive vision monitoring and accelerated clinical trials aimed at stemming retinal diseases.
The project brought together biomedical engineers, physicists and clinical scientists from the Singapore Eye Research Institute, Nanyang Technological University and the University of Washington.
Funders of the research included the U.S. National Institutes of Health (U01EY032055, EY029710), Research to Prevent Blindness, the George and Martina Kren Professorship in Vision Research, Dawn’s Light Foundation, and the Kren Engineering-based Medicine Initiative.
Dedicated ORs for Ophthalmology open at Harborview
After five years of planning, the dream of having dedicated outpatient operating rooms for the Department of Ophthalmology has become a reality.
Five operating rooms on the fourth floor of the Ninth and Jefferson Building opened Jan. 6, two of which are dedicated full-time to Ophthalmology. This is the same building that houses the Eye Institute on the seventh floor.
“We have always desired to have outpatient surgeries in a dedicated outpatient setting,” said Associate Professor and Medical Director of Surgical Services Kasra Rezaei, MD. “This is a great opportunity to improve our workflow and enhance patient care.”
The two new ORs, designed for ophthalmology, will allow 90 percent of the current surgery cases in the Maleng Building across the street to be moved to NJB. They will share a pre-anesthesia clinic, post-anesthesia care unit, and waiting room.
“This will help us to improve efficiency and create the ability to do more cases,” Dr. Rezaei said. “It will be much easier for patients to receive their surgical and clinical care in the same building.”

Jeff Dabundo, OD, joins faculty as triage optometrist
Dr. Jeff Dabundo, OD, has joined the faculty as a Rapid Access (Triage) Optometrist and Teaching Associate.

As a triage optometrist, Dr. Dabundo joins the UW Medicine Eye Institute to help provide urgent eye care to patients with new-onset ocular symptoms and to appropriately refer them to ophthalmology specialty care, as needed.
“This is such an exciting enhancement for our patients and our outpatient triage service,” said Ian Lutrell, Director of Program Operations for the Eye Institute.
Dr. Dabundo earned his B.S. in neuroscience from Washington State University before completing his optometric training at Pennsylvania College of Optometry in Philadelphia. There, he also completed postgraduate optometric training at Wills Eye Hospital and Philadelphia VAMC, working with Jefferson and UPenn ophthalmology, respectively. He then completed his optometric training in ocular disease in Wilmington, DE, at the Wilmington VAMC, working with Temple University ophthalmology.
Prior to joining the UW Eye Institute at Harborview, Dr. Dabundo practiced optometry in private practice in the Seattle area, providing comprehensive eye care to diverse patient populations.
Outside of work, he enjoys exploring the Pacific Northwest via hiking, skiing, and general aviation as a private pilot.
Jeannette Stallworth, MD joins faculty as Assistant Professor
Jeannette Stallworth, MD, returned to UW Ophthalmology in January as an Assistant Professor on the pediatric ophthalmology team at Seattle Children’s.
A Bellevue native, Dr. Stallworth spent the 2023-24 year as the department’s Pediatric Fellow. She graduated from Newport High School before attending Princeton University, graduating magna cum laude with a Bachelor of Arts in Economics. She earned her medical degree from Duke University School of Medicine and completed her general surgery internship and ophthalmology residency at the University of California, San Francisco.
She worked at the Pediatrix/Children’s Eye Care clinic in Kirkland after completing fellowship.
Her research interests focus on retinopathy of prematurity. When many newborns are born prematurely, they are at risk for Retinopathy of Prematurity (ROP), a disease of the developing retina.
Outside of work, Dr. Stallworth enjoys playing the cello, traveling, and spending time with her husband and two children.
Meet our new fellows for 2026-27
Match Day for fellowships was held recently, and the following have matched with the UW Department of Ophthalmology:
Glaucoma
Raj Patel, MD
Residency: University of Missouri – Kansas City
Neuro-Ophthalmology
Scott Sorenson, MD
Residency: California Pacific Medical Center – San Francisco
Ocular Oncology (new fellowship for 2026)
Alyssa Bonnell, MD
Residency: University of Washington
Fellowship: University of Washington (Medical and Surgical Retina)
Pediatrics
Elizabeth Noh, MD
Residency: University of Arizona - Tucson
Retina
David Mundy, MD
Residency: University of Michigan
Uveitis (Two-Year Program)
Behrouz Rahimi, MD
Residency: Isfahan University of Medical Science
Fellowship: Shahid Beheshti Medical University (Ophthalmology)
Etti Katzburg, MD
Residency: Tel Aviv Medical Center
Fellowships: Moran Eye Center (Medical Retina), Tel Aviv Medical Center (Medical Retina)
Our current fourth-year residents matched into the following fellowships:
Amanda Hoyer, MD—Pediatrics, Northwestern Lurie
Grant Howell, MD—Neuro-ophthalmology, Moran Eye Center
Marcus Toral, MD, PhD—Uveitis, Oregon Health Sciences University
Cameron Ward, MD—Medical Retina, National Eye Institute
Meet our Class of 2030 Residents
We had another successful residency match this year. Please welcome our first class of 6 residents:
Kenneth Han, University of Arizona
Talya Jaffe, University of New Mexico
Mark Lindquist, University of Hawaii
Alexis Monical, University of Chicago
Pul Park, Rutgers Robert Wood Johnson Medical School
Frida Velcani, Geisel School of Medicine at Dartmouth
They’ll start with UW Internal Medicine this upcoming July and will join us as a PGY-2 in July 2027.
Dawn's Light Foundation gift to create new clinical trials space at SLU
Chris and Jenny Carlson have a deeply personal connection to genetic research. Chris spent more than 15 years as a researcher at Fred Hutch Cancer Center, where his work focused on uncovering how genetic variations contribute to common diseases, including cancer, cardiovascular disease, and neurological conditions. That scientific lens became even more meaningful when a family member was diagnosed with an Inherited Retinal Disease (IRD) in 2021. Since then, the Carlsons have dedicated themselves to championing research, expanding access to clinical trials, and strengthening the therapeutics and treatment pipeline for individuals affected by IRDs.
The Carlsons established Dawn’s Light Foundation, named in honor of Jenny’s mother—a woman they lovingly describe as a “guardian of lost causes.” Following their family member’s diagnosis, they felt a renewed urgency to support research that could meaningfully change the future for IRD patients and accelerate the development of new treatments.
During the last two years, their philanthropic leadership has played a pivotal role in advancing IRD research within our department. Building on that momentum, the department recently approached the Carlsons with a vision for a transformative partnership: strengthening our clinical trials infrastructure and expanding the physical and personnel capacity needed to support a rapidly growing research portfolio.
“With the support of the Dawn’s Light Foundation, we have an extraordinary opportunity to transform our clinical trials infrastructure,” said Dr. Russell Van Gelder, Bucey Chair in Ophthalmology. “Clinical trials are the engine of medical advancement, and in recent years our department has seen remarkable growth. Yet our ability to sustain and scale this critical work is increasingly limited by inadequate space and the need for a more robust, adaptable research team.”
Thanks to a transformational gift from Dawn’s Light Foundation in November, a 1,100-square-foot shelled space in the South Lake Union F building—adjacent to research laboratories and one floor above clinic operations—is now being converted into a purpose-built clinical trials center. Opening this summer, the new facility will house up to 10 staff members and optimize patient care, study coordination, and research activities. This enhanced infrastructure will ensure that Ophthalmology’s clinical trials program can continue to pursue cutting-edge discoveries and bring emerging therapies to patients more efficiently.
“Chris and Jenny’s commitment to advancing research and patient care is making a meaningful difference in the lives of those we serve,” said Dr. Van Gelder. “Support like theirs enables us to push the boundaries of innovation and improve outcomes for individuals facing vision loss.”
If you would like to help strengthen our growing clinical trials program, click here to make a gift of support.

InSight Newsletter Fall 2025
InSight Newsletter Fall 2025
Message from the Chair
Welcome to the Fall 2025 edition of the Department of Ophthalmology InSight Newsletter. We are now well into the 2025-26 academic year, and it has been the most unusual – and in many ways challenging – in my almost 18 years as chair. As you are aware, substantial changes in Federal policy have occurred in the past year that have impacted our NIH grant funding and may soon impact our payments for clinical services. In anticipation, the University of Washington is implementing significant austerity measures. Despite this, our research continues at a brisk pace, and we continue to provide outstanding patient care.

Our community’s support has allowed us to continue to fulfill our mission. This issue's research spotlight is on the Kren Engineering-based Medicine Initiative (KEMi). Made possible by an extraordinarily generous gift from George and Martina Kren, emeritus members of our Community Action Board, and catalyzed by fellow emeritus CAB member Graham Siddall, this initiative combines the strengths of UW Engineering and UW Medicine to develop solutions for healthcare’s most urgent unmet needs. KEMi, led by Graham and Brenda Siddall Professor Tueng Shen, MD, PhD, will focus on engineering-driven projects that translate advanced technologies from laboratory research into real-world clinical tools. A substantial portion of this initiative is directed toward ophthalmology research, and we are delighted to feature these projects in this quarter’s newsletter.
In this issue, we also introduce Acting Assistant Professor Yue Wu, PhD, who has taken a leadership role in the Computational Ophthalmology Lab following the departures of Drs. Aaron and Cecilia Lee for leadership positions at Washington University in St. Louis. Dr. Wu has been in our department for more than seven years and has collaborated with many faculty members, including myself, on research projects involving large datasets. We will continue much of the work started by the Lees.
Our Patient Care Spotlight welcomes two terrific physicians to the faculty: Acting Assistant Professor Nathan Agi, MD, and Alexa Van Brummen, MD. Both are staying with us after completing their fellowship specialty training: Dr. Agi in vitreoretinal surgery and Dr. Van Brummen in oculoplastic surgery.
In Education, our department hosts medical students from UW and around the country for summer clerkships each summer. Learn more about Lensa Moen, a student at Washington State University who received a scholarship for her summer experience at Harborview and Seattle Children’s.
Our faculty also mentors several graduate students in their doctoral programs, and recently, Samson Darrah, OD (a PhD student in Dr. Debarshi Mustafi’s lab) received the prestigious Homecoming Scholar Award from the UW Alumni Association.
Finally, in our philanthropy spotlight, learn more about the generosity of our donors and the support of two key initiatives: the Vision Research Innovation Fund and the Tietze Family Award for Vision Sciences. These programs empower junior faculty to pursue groundbreaking, early-stage research with the potential to transform patient care.
Wishing you and yours all the best this upcoming holiday season.
Russ Van Gelder, MD, PhD,
Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Director, Roger and Angie Karalis Johnson Retina Center
Director, Vision Science Center
Research Spotlight:
The KEMi Initiative - Accelerating
Transformative Research
The Kren Engineering-based Medicine Initiative (KEMi) combines the strengths of UW Engineering and UW Medicine to develop solutions for healthcare’s most urgent unmet needs. KEMi is made possible by a generous gift from George and Martina Kren.
KEMi will focus on engineering-driven projects, primarily in Ophthalmology, that translate advanced technologies from laboratory research into real-world clinical tools. Collaborative projects between ophthalmology and engineering will lead the way, drawing on the strong expertise in both areas.
“Engineers, physicians, and medical researchers will work side by side to co-develop tools and technologies that are both technologically advanced and grounded in real patient needs—from early diagnostics to precision therapeutics,” said Bucey Chair and Professor of Ophthalmology Russell Van Gelder, MD, PhD.
“We received an overwhelming response to our call for proposals, with 83 submissions. The committee has selected the projects that will serve as the inaugural group of KEMi investigators,” said Graham and Brenda Siddall Endowed Chair Tueng Shen, MD, PhD. “In the inaugural year of the Kren Engineering-based Medicine Initiative (KEMi), we especially emphasized funding research projects in Ophthalmology."
KEMi is poised to integrate cutting-edge technologies into clinical practice, addressing the growing demand for early detection and more precise treatments. Its interdisciplinary approach ensures that innovations are technologically advanced and rooted in real-world medical needs. As the initiative progresses, its impact will extend across various medical fields, paving the way for broader applications that can reshape the future of healthcare.
The selected proposals are listed below.
Vision-based projects
Advancing Volumetric Phase-Sensitive OCT for Wide-Field Functional Imaging of Trabecular Meshwork Dynamics
Principal investigator: Ruikang Wang, Ph.D., Professor and George and Martina Kren Endowed Chair, Ophthalmology
Leveraging the ADDF and EyeACT Datasets to Learn and Predict Dementia, Identifying Dementia Biomarkers
Principal investigator: Yue Wu, Ph.D., Acting Assistant Professor, Ophthalmology
Early Detection of Photoreceptor Dysfunction in Outer Retinal Disease Using Optoretinography
Principal investigator: Ramkumar Sabesan, Ph.D.,George and Martina Kren Associate Professor, Ophthalmology
Co-principal investigators:
Jennifer Chao, M.D., Ph.D., Joan and Gordon Bergy Professor, Ophthalmology
Debarshi Mustafi, M.D., Ph.D., Assistant Professor, UW Ophthalmology and Seattle Children's Hospital
Wearable Assist Device to Improve Visual Function Following Restorative Therapy
Principal investigator: James A. Kuchenbecker, Ph.D., Acting Assistant Professor, Ophthalmology
Co-principal investigators:
Russell Van Gelder, M.D., Ph.D., Boyd K Bucey Memorial Professor and Chair, Ophthalmology
Ruikang Wang, Ph.D., Professor and George and Martina Kren Endowed Chair, Bioengineering
Injectable Biomaterial-Mediated Transplantation of Limbal Fibroblasts for Treatment of Limbal Stem Cell Deficiency
Principal investigator: Yuzuru Sasamoto, M.D., Ph.D., Assistant Professor, Ophthalmology
Co-principal investigator: Cole DeForest, Ph.D., Associate Professor, Bioengineering
Kren-Endowed chair project
High-Resolution Facial Imaging for Non-Invasive Detection of Rhythm Irregularities and Perfusion Deficits in Atrial Fibrillation Patients
Principal investigator: Nazem Akoum, M.D., M.S., FACC, FAHA, FHRS, Professor of Medicine, Cardiology
Co-principal investigator: Ruikang Wang, Ph.D., Professor, Bioengineering
For a complete list of the funded proposals, visit the KEMi website.

Research Spotlight:
Yue Wu, PhD, assumes leadership role for Computational Ophthalmology Lab
From Shanghai to Switzerland to Seattle, Dr. Yue Wu has traveled a long way in his life.
Dr. Wu is now leading the Computational Ophthalmology Lab in the Vision Science Center at South Lake Union. This summer, faculty members Aaron and Cecilia Lee, previous leaders of this lab, relocated for new leadership positions at Washington University in St. Louis.
Now an Acting Assistant Professor, Dr. Wu was initially recruited to UW by the Lees in 2017 after completing his PhD in mathematics at the University of Cambridge.
Computational Ophthalmology uses machine learning and data science methods to leverage modern computing and more modern deep learning and AI datasets.
This has included analysis of retinal images to understand how labels for dementia can be determined from these images. Over many years of study, the EYE-ACT studies have found that the eye is almost a biological twin of the brain, detecting retinal biomarkers for dementia, and it can be detected earlier.
The Lees’ major EYE-ACT study and Bridges to AI work will continue at UW under Wu’s leadership and that of Associate Professor Kathryn Pepple, MD, PhD, who also serves as Director of Clinical Research.
Dr. Wu is also working on a significant study of Macular telangiectasia (MacTel), a rare eye disorder affecting the macula, the central part of the retina responsible for sharp, central vision.
He collaborates on analyzing data with many faculty members, including Bucey Chair Russ Van Gelder, Dr. Pepple, and Dr. Tim Cherry from Seattle Children’s.
Born in Shanghai, Dr. Wu moved to Switzerland when he was 8 years old. His parents worked as translators for the United Nations in Geneva. He came to the United States for college at Harvard University, receiving a B.A. in Statistics. He went on to Cambridge to earn his PhD in machine learning before joining the Computational Ophthalmology Lab at UW.
“I like solving practical problems. How can we understand patterns that the data gives us?” Dr. Wu said.
In his free time, Dr. Wu enjoys biking and playing squash.

Education Spotlight:
Meet Lensa Moen, Visiting Clerkship Scholar
Each year, the Department of Ophthalmology awards a visiting clerkship scholarship to a fourth-year medical student. A generous donor provided the scholarship.
This past summer, the recipient was Lensa Moen, who attends the Elson S. Floyd College of Medicine at Washington State University in Spokane.

“I am honored and grateful to have been selected as the 2025 recipient of the University of Washington Ophthalmology Visiting Student Scholarship.”
Moen had the opportunity to experience the exceptional education in ophthalmology at UW, spending four weeks at Harborview Medical Center and Seattle Children’s.
Lensa was born in Ethiopia and later emigrated to Sweden with her family. She is multilingual, speaking two Ethiopian languages and Swedish fluently in addition to English.
She came to UW for college, studying neuroscience, then completed a one-year post-baccalaureate clinical internship in medical lab science. She was a medical technologist for 10 years before entering medical school. She is married and the couple had their first child last year.
She became interested in ophthalmology first when a friend had a retinal detachment, and saw how he received immediate, vision-saving treatment for that.
She asked to be placed with an ophthalmologist for a rotation, “and I was hooked after seeing my first surgery.”
During her visiting clerkship this summer, she particularly enjoyed working with the ophthalmology physicians at Seattle Children’s.
“I marveled at their ability to determine eyeglass prescriptions for non-verbal children using retinoscopy,” Moen said.
“I am hoping to be married to ophthalmology,” she said. “I am proposing (applying to residency programs) and we’ll see if she says yes.”
Samson Darrah, OD, honored as Homecoming Scholar by UWAA
Each year, the UW Alumni Association is proud to honor six exceptional students across the UW’s Seattle, Bothell, and Tacoma campuses whose stories exemplify Husky adaptability, tenacity, and resolve. Each student is awarded a $6,000 scholarship and recognized at the Homecoming football game in the Fall.
Samson Darrah, OD, is a PhD student in Bioengineering whose research bridges high-resolution ophthalmic imaging and genetics to better understand retinal diseases. He is being mentored by Assistant Professor Debarshi Mustafi, MD. PhD and Kren Associate Professor Ram Sabesan, PhD.
He was recently honored to become a Fellow of the American Academy of Optometry (AAO). Fellowship in the AAO is one of the highest professional honors in the field of optometry and vision science. It is conferred on individuals who have demonstrated exceptional competence, dedication, and contributions to advancing eye and vision care through clinical practice, research, education, or public service.
Dr. Darrah is passionate about building community for international and underrepresented students at the UW. Samson mentors students navigating research and scholarships, drawing from his journey to help them build confidence and access opportunities he once struggled to find. He also leads global health outreach through iCare Network International, a nonprofit he founded to expand access to vision care in underserved communities. Samson aims to make science more inclusive and improve health equity worldwide through research, mentorship and service.

Philanthropy Spotlight: Fueling the Future of Vision Science: Supporting Innovation and Discovery
The Department of Ophthalmology is driving bold new discoveries in vision science, thanks to the generosity of our donors and the support of two key initiatives: the Vision Research Innovation Fund and the Tietze Family Award for Vision Sciences. These programs empower junior faculty to pursue groundbreaking, early-stage research with the potential to transform patient care.
The Vision Research Innovation Fund, established by members of the Community Action Committee, supports investigations across scientific, technical, and humanistic dimensions of vision science—leading to meaningful advances in diagnostics, therapies, and care models. Each year, one faculty member is honored with the Latham Endowed Faculty Fellowship for Vision Research Innovation, a distinction that recognizes their promise and provides essential resources to advance their work. This fellowship was made possible through the generosity of Community Action Board members Alida and Chris Latham, whose vision elevated the fund into a powerful catalyst for discovery.
In parallel, the Tietze Family Award for Vision Sciences celebrates exceptional early-career researchers whose innovative work is pushing the boundaries of understanding and improving eye health. This award was made possible by John and Eileen Tietze, whose support ensures that promising faculty have the resources to explore bold ideas and make meaningful contributions to vision science.
Projects supported through these initiatives showcase the depth and promise of discovery across the department. Past investigations include:
- Exploring strategies to slow the progression of myopia in children and adolescents.
- Using advanced imaging to detect retinal changes associated with Alzheimer’s disease.
- Improving the accuracy of eye exams in emergency settings following blunt ocular trauma.
- Examining the effects of chronic circadian disruption on inherited retinal degeneration in animal models.
Each study reflects the creativity and dedication of our junior faculty as they push the boundaries of vision science—to improve lives and shape the future of eye care.
None of this progress would be possible without the generosity of our donors. Thanks to the Lathams, the Tietzes, our Community Action Board members, and all who support these awards. Because of you the next generation of scientists and clinicians has the resources and encouragement to dream boldly, tackle urgent challenges, and bring hope and healing to patients and families around the world.
Be part of nurturing bold ideas and discoveries in vision science with the Vision Innovation Awards. - Vision Research Innovation Award.
VRI Awards for 2025 – 2026
Minh Nguyen, Assistant Professor – “Cell-Free DNA in Tear Fluid as a Non-Invasive Biomarker for Ocular Surface Squamous Neoplasia and Conjunctival Melanoma.”
Kathryn Pepple, MD, PhD, Associate Professor – “Ocular immunology collaborative biorepository.”
Karine Duarte Bojikian, MD, Assistant Professor and Eric Duerr, MD, Assistant Professor
“Incidence of Neovascular Glaucoma in Diabetic and Retinal Vascular Occlusive Disease Eyes Treated with Anti-VEGF Monotherapy Versus Panretinal Photocoagulation in the American Academy of Ophthalmology IRIS® Registry.”
Rayne R Lim, PhD – “Investigating the non-canonical role of the complement pathway component C3 in the RPE.”
InSight Newsletter Summer 2025
InSight Newsletter Summer 2025
Message from the Chair
Welcome to the Summer 2025 edition of the Department of Ophthalmology InSight Newsletter. We are beginning the 2025-26 academic year, as our incoming first-year residents begin training and our new fellows join us. We salute our class of 2025 as they leave us for private practice or specialty training.
This issue's research spotlight shines on the work of Assistant Professor Chris Fortenbach, MD, PhD. Dr. Fortenbach has been awarded a Career Development Award from Research to Prevent Blindness (RPB). RPB is a leading nonprofit organization supporting eye research directed at the prevention, treatment or eradication of all diseases that threaten vision. Our department has been fortunate to receive support fromRPB for many decades to support our research.
Dr. Fortenbach is investigating the therapeutic potential of small molecule photoswitches to restore vision in degenerated retinas in his lab at the Vision Science Center at South Lake Union. These light-sensitive small molecules bind to the degenerating retina and confer new light sensitivity to surviving retinal cells. Several generations of these molecules have been developed with differing cell target specificity and sensitivity.
Our Patient Care Spotlight features the Uveitis Division, among the largest in the country. The uveitis team of five faculty and one fellow, headed by Associate Professor Kathryn Pepple, MD, PhD, provides specialized eye care to patients of all ages throughout the region. Dr. Pepple is a clinician-scientist with an active lab in the Vision Science Center at South Lake Union, where she sees patients at the Karalis Johnson Retina Center. Her research and clinical efforts address her central career goal of preventing blindness in her patients with uveitis through effective management of ocular inflammation.
In Education, our class of 2025 of residents and fellows was honored at the graduation dinner on June 14. We are so proud of them and welcome them to our ranks of UW Ophthalmology alumni.
Finally, in our philanthropy spotlight, please enjoy this story and video created by our Advancement team about Community Action Board member Jack Odell, a patient of ocular oncologist Associate Professor Andrew Stacey, MD.
UW Ophthalmology’s ocular oncology program is one of the few in the country with specialized expertise in these rare and often aggressive conditions. Patients have access to the latest, most effective options, including surgery, advanced radiation therapies and precision medicine approaches that tailor treatments to individual needs.
To one patient, Jack Odell, a member of our Community Action Board, Dr. Stacey and his team are a powerful reminder of how life-changing this care can be. Watch the video below to learn more about Mr. Odell's journey with uveal melanoma and how he is helping others.
Wishing you and yours all the best this summer.
Russ Van Gelder, MD, PhD,
Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Director, Roger and Angie Karalis Johnson Retina Center
Director, Vision Science Center
Research:
Chris Fortenbach, MD, PhD, receives RPB Career Development Award
Chris Fortenbach, MD, PhD, Assistant Professor in the UW Department of Ophthalmology, has been awarded a Career Development Award from Research to Prevent Blindness (RPB).
This is one of RPB’s flagship awards, and provides outstanding early-career vision scientists with significant support to start and sustain an independent research program. The $350,000 grant provides support over four years.
Research to Prevent Blindness (RPB) is a leading nonprofit organization supporting eye research directed at the prevention, treatment or eradication of all diseases that threaten vision. RPB-supported researchers have been associated with many breakthroughs in the understanding and treatment of vision loss over the past 65 years.
Among the leading causes of vision loss, outer retinal degeneration impacts millions of people worldwide. These diseases, such as age-related macular degeneration and retinitis pigmentosa, are characterized by the death of rod and cone photoreceptors, resulting in declining vision and, in some cases, blindness. Once photoreceptors have been lost, there are no current treatments to restore vision.
Dr. Fortenbach is investigating the therapeutic potential of photoswitches to restore vision in degenerated retinas in his lab at the Vision Science Center at South Lake Union. These light-sensitive small molecules bind to the degenerating retina and confer new light sensitivity to surviving retinal cells. Several generations of these molecules have been developed with differing cell target specificity and sensitivity.
In contrast to other therapies requiring surgery, photoswitches can be delivered via intravitreal injection, a procedure performed over 20 million times per year globally. Most recently, promising phase 1 clinical trial data have demonstrated vision restoration in several human subjects.
The Fortenbach Lab is researching the mechanisms by which photoswitches restore light sensitivity and methods to improve visual outcomes among treated individuals. The lab uses a combination of electrophysiology methods, including whole-cell and multielectrode array recordings, in conjunction with machine learning to assess the ability of photoswitches to encode visual information. Overall, the lab’s goal is to help develop a medication capable of restoring sight and improving the quality of life for patients with vision loss.
Dr. Fortenbach joined the faculty in August 2023 after completing his ophthalmology residency and vitreoretinal surgery fellowship at the University of Iowa Hospitals and Clinics. His clinical practice is at the Karalis Johnson Retina Center and the Veterans Affairs Puget Sound Healthcare System.
The UW Department of Ophthalmology receives an unrestricted departmental grant annually from RPB. Past UW Ophthalmology recipients of RPB career development awards include Jennifer Chao, MD, PhD; Aaron Lee, MD; Jay Neitz, PhD; Maureen Neitz, PhD; Kathryn Pepple, MD, PhD; Ram Sabesan, PhD, and Russ Van Gelder, MD, PhD.
Since it was founded in 1960, RPB has funded more than $429 million of eye research. RPB has been identified with nearly every major breakthrough in vision research in that time, For information for RPB's grants program, listing of RPB institutional and individual grantees, and findings generated by these awards, visit rpb.usa.org.
Patient Care Spotlight: Uveitis
The UW Department of Ophthalmology has one of the country's most extensive patient care programs for treating uveitis and ocular inflammation.
Uveitis is any form of inflammation that impacts the eye, whether from an infection or autoimmune disease that is limited to the eye or can affect other parts of the body.
“As ophthalmologists, uveitis is a rewarding career because it provides the opportunity to develop a long-term relationship with our patients as we work to determine the cause of their eye condition and how we are going to treat it,” said Associate Professor Kathryn Pepple, MD, PhD, Division Director of Uveitis.
Dr. Pepple is joined in the uveitis division by Bucey Chair and Professor Russ Van Gelder, MD, PhD, Professor of Clinical Practice Thellea Leveque, MD, MPH, Assistant Professor Miel Sundararajan, MD, and Assistant Professor Laura Huang, MD. Thanks to the generous support of the Gensheimer family, the uveitis division also trains one fellow each year. This year, Fatma Dihowm, MD, MS, is one of only about a dozen ophthalmologists training to become uveitis specialists across the entire United States.
“Patients can develop uveitis at any age. Here at UW we can provide care across their life span,” Dr. Pepple said. “For our youngest patients, we are very fortunate to have a dedicated pediatric uveitis specialist in Dr. Laura Huang; very few places can provide this level of dedicated ultra-subspecialized care.”
Dr. Pepple said many patients will come to see them after noticing blurred vision or red eyes, and they will have been given something for pinkeye.
“If they don’t get better, they may see a comprehensive ophthalmologist, and when that treatment fails, they are referred to us for specialty care. It’s not uncommon for patients to experience a delay between symptom onset and final diagnosis of uveitis.”
Uveitis can be challenging because there is no one-size-fits-all treatment.
“Some eye drops may be useful for some people, but others might need more advanced treatment with anti-inflammatory medications that they take by mouth or injections under the skin. Alternative treatments can also include injections into the eye to control the inflammation,” Dr. Pepple said. “Sometimes uveitis is caused by a systemic autoimmune condition that people may have heard of before, like lupus, arthritis, or inflammatory bowel disease. But over half the time, we don’t identify a problem outside of the eye.
“Regardless of cause, as uveitis specialists, we can help prevent patients from losing vision from uveitis by treating the inflammation. Treatment is the key to preventing blindness, as untreated uveitis is one of the leading causes of blindness in working-age people.”
Dr. Pepple is a clinician-scientist with an active lab in the Vision Science Center at South Lake Union, where she sees patients at the Karalis Johnson Retina Center. Her research and clinical efforts address her central career goal of preventing blindness in her patients with uveitis through effective medical management of ocular inflammation.
“Having that long-term relationship with my patients to keep their vision, combined with the research, is so important, and there is so much left to learn,” said Dr. Pepple.
She is launching a new research project in collaboration with the University of Colorado and Oregon Health Sciences University to develop a multi-center biorepository of samples of uveitis to study inflammatory responses in the eye.
“Hopefully, this study will help us understand the specific types of uveitis better and help us choose which medicine is best for each patient,” Dr. Pepple said.
She has been joined for this research by post-doctoral scholar Rachel Van Gelder, PhD, who recently completed her doctorate in immunology.
Dr. Pepple’s research has been supported by grants from the National Institutes of Health, Foundation Fighting Blindness, Research to Prevent Blindness, and generous gifts from donors, including Graham and Brenda Siddall and Mark J. Daily, MD.

Faculty honored as among Top Doctors 2025 by Seattle Magazine
UW Medicine Ophthalmology faculty members have been honored as among Seattle’s Top Docs 2025 by Seattle Magazine in its July 2025 issue. Seattle Magazine has published a list of the region’s top doctors for the past 25 years. None paid to be included, and all were nominated by their peers.
UW Ophthalmology faculty honored as Top Docs by Seattle Magazine are:
Michelle Cabrera, MD (pediatrics); Professor; Division Director, Pediatric Ophthalmology
Christopher Chambers, MD (oculoplastics); Professor; Division Director, Oculoplastic and Reconstructive Surgery
Philip Chen, MD (glaucoma); Professor; Grace E. Hill Endowed Chair; Vice Chair for Clinical Services, Chief of Ophthalmology, Harborview Medical Center
Eric Duerr, MD (comprehensive and glaucoma); Assistant Professor
Shu Feng, MD (comprehensive), Associate Professor; Director of Medical Student Education
Courtney Francis, MD (neuro-ophthalmology); Professor; Division Director, Neuro-Ophthalmology; Medical Director, UW Medicine Eye Institute
Eugene May, MD (neuro-ophthalmology); Professor of Clinical Practice
Raghu Mudumbai, MD (glaucoma and neuro-ophthalmology); Associate Professor; Division Director, Glaucoma
Miel Sundararajan, MD (cornea and external disease and uveitis), Assistant Professor, Division Director, Cornea and External Disease
Russell Van Gelder, MD, PhD (uveitis); Boyd K. Bucey Memorial Professor and Chair, UW Medicine Department of Ophthalmology; Director, Roger and Angie Karalis Johnson Retina Center; Director, UW Vision Science Center
Jennifer Yu, MD, PhD (comprehensive); Professor of Clinical Practice; Director, 4W Ophthalmology Clinic at Harborview; Director of Trauma and Consult Services at Harborview
Education Spotlight:
Residents, fellows honored at annual dinner
Five residents and four fellows were honored at the annual graduation dinner, which was held on June 14 at the Women’s University Club in Seattle.
The graduation event honored fellows Nathan Agi, MD (Retina), Gunay Kirimli, MD (Uveitis), Alexandra Van Brummen, MD (Oculoplastics), and Menatullah Elfwaal, MD (Pediatrics). Drs. Agi and Van Brummen are joining the faculty later this year.
The graduating residents are Sam Kushner-Lenhoff, MD (retina fellowship, UC Davis), Nicole Mattson, MD (glaucoma fellowship, Univ. of Iowa), Zesemayat Mekonnen, MD (private practice, California), Gayathri Tummala, MD (private practice, California), and Ryan Yanagihara, MD (medical retina fellowship in Texas) . Dr. Tummala received the Resident Research Award
Assistant Professor Miel Sundararajan, MD, was honored as the faculty teacher of the year. Michael Brush, MD, was honored as the volunteer of the year. Allein Siwa of the Eye Institute was honored as the staff person of the year. The graduating residents chose these recipients. Third-year resident Johnson Huang, MD, received the Academic Excellence Award, and Najma Adan, MD, received the Medical Student of the Year award.

Philanthropy: Research leads to new treatments for patients with rare eye cancers
(from UW Medicine Advancement, read the entire story here.
Uveal melanoma, also known as ocular melanoma, is rare; only a few thousand individuals are diagnosed every year. This aggressive cancer and its treatments often lead to vision loss and a high rate of secondary metastasized cancer.

UW Medicine is transforming how we treat eye cancers, offering patients a brighter future and new possibilities for longer, healthier lives.
“At UW Medicine, we have world-class physicians and world-class facilities, which allows us to bring patients with rare tumors to one place that is quite unique in the country. It creates an opportunity for a center of excellence that is unmatched,” says Associate Professor of Ophthalmology Andrew Stacey, MD, MSc.
Dr. Stacey — who is the first and sole ocular oncology-focused surgeon for the Washington, Wyoming, Alaska, Montana and Idaho region — joined UW Medicine in 2016, launching the region’s only full-service comprehensive eye cancer unit at the UW Medicine Eye Institute at Harborview Medical Center.
UW Ophthalmology’s ocular oncology program is one of the few in the country with specialized expertise in these rare and often aggressive conditions. Patients have access to the latest, most effective options available, including surgery, advanced radiation therapies and precision medicine approaches that tailor treatments to individual needs.
As a leader in ocular cancers, UW Medicine is able to engage in groundbreaking research and select studies that can advance the standard of care, providing patients with access to cutting-edge treatments before they are widely available.
To one patient, Jack Odell, Dr. Stacey and his team are a powerful reminder of how life-changing this care can be. Learn more about Mr. Odell's journey with uveal melanoma and how he is helping others in this video.
InSight Newsletter Spring 2025
InSight Newsletter Spring 2025
Message from the Chair
Welcome to the Spring 2025 edition of the Department of Ophthalmology InSight Newsletter. We are nearing the end of the 2024-25 academic year, as our class of 2025 residents and fellows prepare to graduate, and we look forward to welcoming our incoming class of residents and fellows in July.
This issue's research spotlight shines on the research of Professor Lisa Olmos de Koo, MD, MBA. Dr. Olmos de Koo has been collaborating with colleagues worldwide on retinal prostheses research for nearly 15 years. The current device she is working with has shown promising results in clinical trials for restoring vision to individuals who have become blind from retinal disease.
Our Patient Care Spotlight features the growing Pediatric Ophthalmology division, based at Seattle Children’s. The pediatric team, headed by Professor Michelle Cabrera, MD, provides specialized eye care to children from throughout the region.
In Education, our residents again volunteered to help the uninsured and underserved at the annual Seattle/King County Clinic at Seattle Center, part of our community outreach efforts led by Assistant Professor Miel Sundararajan, MD. It is the largest community-driven, free health clinic of its kind in the United States, and we are honored to participate in it each year.
Finally, in our philanthropy spotlight, Clinical Associate Professor Emeritus Dr. Richard “Rick” Munsen and his wife, Deidra Wager, together with generous support from a small group of grateful patients, have established the Richard S. Munsen, M.D. Professorship in Ophthalmology. This endowed position recognizes Dr. Munsen’s extraordinary legacy as a retina specialist, educator, and humanitarian.
If you haven’t seen our 2024 Community Report, it is available on our website here. For more news and updates, please visit our website, Facebook, Instagram, and LinkedIn pages.
Wishing you and yours all the best this spring.
Russell N. Van Gelder, MD, PhD,
Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Director, Roger and Angie Karalis Johnson Retina Center
Director, Vision Science Center
Research: PRIMA implant shows promise
Research is making substantial progress in the use of retinal prostheses to restore vision in patients who are blind due to photoreceptor loss in degenerated retinas.
Retinal prostheses electronic devices that deliver electrical stimulation to the blind retina, inducing “artificial vision.” To date, three retinal prostheses have been approved for implantation outside of clinical trials, all of which are targeted at patients with retinitis pigmentosa.
UW Professor of Ophthalmology Lisa Olmos de Koo, MD, MBA, has been working on retinal prosthesis research for nearly 15 years, dating back to the original ‘Argus II’ device developed in Southern California. More recently, she has been working with an international team based at Stanford University developing the PRIMA prosthesis. She notes that a recent large clinical trial in Europe has yielded promising results for the device.
“Use of retinal prostheses has a strong upside,” Dr. Olmos said. “The large research pipeline offers hope for future advances in retinal prosthesis design and vision restoration for those blinded by photoreceptor loss. We are hoping to achieve vision restoration for those patients who don’t have any other options because of geographic atrophy.”
Geographic atrophy (GA) is an advanced form of dry macular degeneration characterized by the death (or atrophy) of cells in the central part of the retina, known as the macula.
“For many patients with GA, this is the only thing we can offer at present in terms of getting vision back,” Dr. Olmos said.
Dr. Olmos de Koo is collaborating with researchers at Stanford University and other institutions on the new device, which is designed to aid individuals blinded by dry age-related macular degeneration with geographic atrophy.
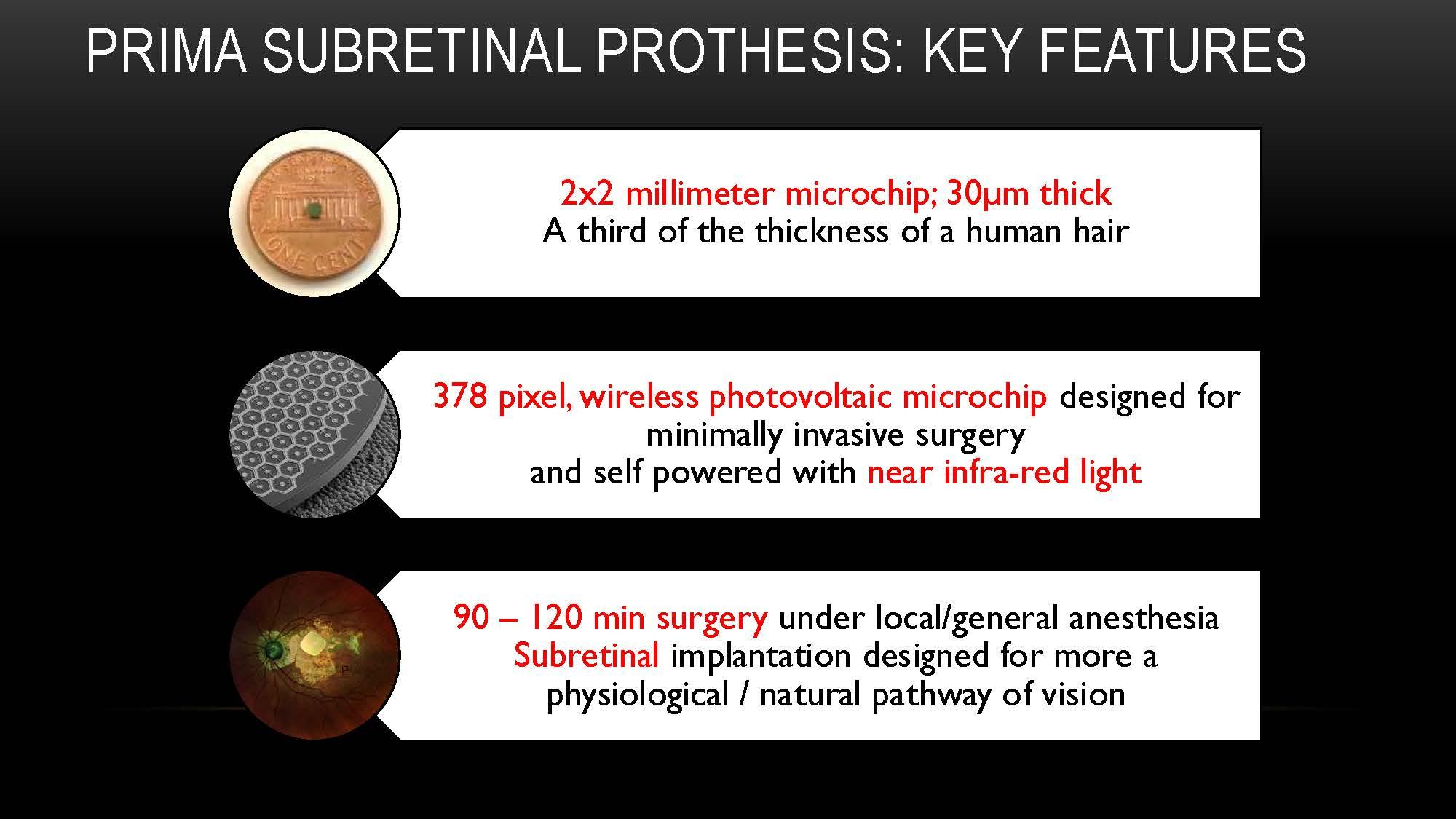
The PRIMA is a wireless, subretinal, photovoltaic microchip that is approximately one-third the thickness of a human hair and utilizes a near-infrared light source to power the implant. The nanoelectrodes stimulate remaining cells in the degenerated retina to induce visual phenomena. Once surgically implanted, the patient operates the device using a pocket-sized processor and wears specialized glasses equipped with a video camera. It is being developed by Science Corporation. The pivotal clinical trial of the device, known as the PRIMAvera study, involved 38 patients, primarily in Europe.
Patients in the clinical trials experienced significantly improved visual acuity with the PRIMA device.
PRIMA produces the best prosthetic visual acuity to date, Dr. Olmos de Koo said. Patients can use the device for reading letters, numbers, and words. Some patients can even read longer text. Dr. Olmos de Koo is a consultant to Science Corporation, which is developing the device and hopes to bring it to the U.S. market.
Remembering Clinical Professor Murray Johnstone, PhD
Murray Johnstone, MD, Clinical Professor of Ophthalmology for the past 15 years, passed away on April 11 at age 86.
“Murray was a true gentleman and beloved by generations of patients. As a colleague, he was an endless source of good humor coupled with a phenomenal drive to understand complex science completely,” said Bucey Memorial Chair and Professor Russ Van Gelder, MD, PhD. “He was an outstanding mentor to a number of our faculty. His dedication to our profession and vision science was truly exemplary, and we will greatly miss his great collegiality.”
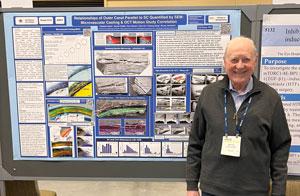
Dr. Johnstone was a native of the Pacific Northwest and attended college at the University of Puget Sound, followed by medical school at Washington University in St. Louis. After completing internship at Harborview, Murray completed his ophthalmology residency and glaucoma fellowship at Mass Eye and Ear Infirmary/Harvard Medical School.
During fellowship, Dr. Johnstone did research in the Howe lab under the tutelage of glaucoma pioneer Morton Grant, MD, which stimulated a lifelong passion for understanding ocular fluid dynamics. He returned to Seattle in 1973 and subsequently founded Glaucoma Consultants Northwest, the pre-eminent glaucoma practice in the Seattle area.
Dr. Johnstone’s passion for research remained bright, and he secured NEI funding for his ultrastructural studies of the trabecular meshwork even while running a busy private practice. Murray retired from clinical practice in 2009 and joined the UW Ophthalmology faculty as a Clinical Professor in 2010, where he continued his research on the mechanisms of trabecular outflow.
His scientific accomplishments are numerous. He established a dynamic model for trabecular mesh outflow, widely viewed as foundational for understanding aqueous outflow from the eye. His seminal papers from his time working with Dr. Grant have been cited hundreds of times, and over a dozen of his papers have been cited 100 times or more in the literature (and are still being cited).
Dr. Johnstone made the seminal observation that prostanoid glaucoma drops induce growth of the eyelashes. He patented this finding (US Patent 6,262,105), which was central to developing the glaucoma medication Latisse. After joining the faculty, he continued his cutting-edge research on trabecular outflow, developing a phase-OCT method for visualizing trabecular outflow with colleague Professor and Kren Chair Dr. Ricky Wang.
Dr. Johnstone was a charter member of the American Glaucoma Society (and was honored as the AGS keynote lecturer in 2006 and with the AGS Innovator Award in 2022), was involved in establishing the glaucoma surgery curriculum at the American Society of Cataract and Refractive Surgery, was a frequent course instructor at American Academy of Ophthalmology, earned the Senior Honor Award of the Academy, and gave numerous named lectures throughout the country.
Within the department, he served on the Ophthalmology Technology Assessment Committee and shared his knowledge of technology commercialization with our faculty. Dr. Johnstone and his wife Jeannie have been generous donors to the Department of Ophthalmology. They have supported travel grants for residents to attend scientific meetings and the Murray and Jeanie Johnstone Travel Grant at ARVO.
Patient Care: Pediatric Ophthalmology at Seattle Children's
On a typical Monday morning at Seattle Children’s Ophthalmology Clinic, UW Professor of Ophthalmology and Division Director of Pediatric Ophthalmology Michelle “Mimi” Cabrera, MD, treats a baby born early with retinopathy of prematurity, a high schooler with glaucoma, and a young girl with a blocked tear duct.
“It just shows the breadth of the patients and the conditions we treat here every day,” Dr. Cabrera said. “The kids inspire us; there is so much joy here.”
The UW pediatric ophthalmology team provides comprehensive eye care to children at Seattle Children’s main hospital campus in Laurelhurst, as well as two satellite clinic locations in Bellevue and Everett.
The team includes Dr. Cabrera and comprehensive pediatric ophthalmologists Fran Baran, MD, Erin Herlihy. MD, Laura Huang, MD, and Kristina Tarczy-Hornoch, MD, D.Phil. They are joined by other UW ophthalmology faculty pediatric subspecialists Chris Chambers, MD (Oculoplastics), Debarshi Mustafi, MD, PhD (Pediatric Retina), Andrew Stacey, MD (Ocular Oncology), as well as Vivian Manh, OD (Optometry). They also have a pediatric ophthalmology fellow, currently Mennatullah Elfwwal, MD. They anticipate adding another pediatric ophthalmologist and a physician assistant this year.
“The pediatric ophthalmology practice here at Seattle Children’s has grown tremendously over the 10 years I have been here,” Dr. Cabrera said. The clinic at Seattle Children’s saw more than 7,500 patients in 2024.
The growth stems in part from patients coming from the five-state region for pediatric ophthalmology care.
“We get patients coming to us from elsewhere in Washington, plus Alaska, Idaho, Montana and Wyoming seeking specialized pediatric ophthalmic care not available in their communities,” Dr. Cabera said.
The clinic offers a range of tests, including electroretinograms, oculomotor (eye movement) testing, visual evoked potential, handheld optical coherence tomography (OCT), and genetic testing for inherited retinal diseases.
The pediatric division also has specialized multidisciplinary clinics in collaboration with the rheumatology and neurology departments at Seattle Children’s.
Cabera has an active research lab studying retinopathy of prematurity, a disease of the developing retina, using handheld Optical Coherence Tomography (OCT). An investigational swept-source handheld OCT was developed in the laboratory of Professor Ricky Wang, PhD.
Collaborative efforts with Dr. Wang's lab have allowed her to investigate retinal findings in infants with unprecedented precision, speed, and imaging resolution.
Dr. Cabrera has been Head of Ophthalmology at Seattle Children’s since 2020. She completed her undergraduate degree in biological sciences at Stanford University, followed by Medical School and ophthalmology residency at UCSF. She then pursued a clinical and research fellowship in pediatric ophthalmology and strabismus at the Duke Eye Center, followed by a position at the University of North Carolina at Chapel Hill, before relocating to Seattle.
To learn more about the Pediatric Ophthalmology Clinic, visit their website. To support the work of Dr. Cabrera and others, consider giving to the Pediatric Ophthalmology Research Fund.

Education/Outreach: residents provide vision care to patients at annual Seattle/King County Clinic
Department of Ophthalmology residents participated in the opening day of the @seattlekingcountyclinic at Seattle Center on April 24. The residents and Assistant Professor Miel Sundararajan. MD provided vision screenings to dozens of patients.
UW Medicine Department of Ophthalmology residents participated in Thursday's opening day of the Seattle-King County Clinic at Seattle Center. The residents and Assistant Professor Miel Sundararajan provided vision screenings to dozens of patients.
Seattle/King County Clinic brings together healthcare organizations, civic agencies, nonprofits, businesses, and volunteers to produce the largest community-driven free health clinic of its kind in the United States.
With the help of thousands of volunteers, this four-day clinic transforms facilities on Seattle Center’s campus, normally used for performances and events, into a fully functioning healthcare operation offering dental, vision, and medical care to anyone who struggles to access and/or afford these services.
As a low-barrier clinic, patients do not need to provide any documentation or proof of income, insurance, or immigration status to receive care. Each year, 3,000+ people in need are seen on a first-come, first-served basis.
Philanthropy: Advancing the Future of Retina and Eye Care: The Richard S. Munsen, M.D. Professorship
To honor a career defined by compassion, clinical excellence, and mentorship, Dr. Richard S. Munsen and his wife, Deidra Wager, together with generous support from a small group of grateful patients, have established the Richard S. Munsen, M.D. Professorship in Ophthalmology. This endowed position recognizes Dr. Munsen’s extraordinary legacy as a retina specialist, educator, and humanitarian. Throughout his career, he has positively impacted countless lives by his dedication to preserving sight and mentoring the next generation of ophthalmologists.
Dr. Munsen began his practice in Seattle in 1980 at the Eye Clinic of Seattle and went on to become the founding partner of Vitreoretinal Associates in 1982, where he practiced until 2006. That same year, he joined the University of Washington Department of Ophthalmology as a clinical assistant professor and clinician at the UW Medicine Eye Institute, where he saw patients two days a week and spent the rest of his time performing surgeries and mentoring medical trainees. In 2011, Dr. Munsen played a key role in establishing the Community Advisory Board for the Eye Institute, helping strengthen ties between the clinic and the broader community.
Beyond his work in Seattle, Dr. Munsen volunteered in China and with the Himalayan Cataract Project’s Cure Blindness initiative in Nepal, performing surgeries while teaching local physicians in real-time. These global efforts reflect his deep belief in the power of shared knowledge to improve care and expand access to vision-saving treatment around the world.
The Richard S. Munsen, M.D. Professorship is designed to support retina clinician-scientists who, like Dr. Munsen, are committed to balancing patient care, academic research, and medical education. By investing in emerging leaders in retinal care, the fund ensures that Dr. Munsen’s values—compassion, excellence, and service—continue to shape the future of ophthalmology. The gift he and Deidra Wager have made is a celebration of a life dedicated to healing and teaching, and it opens new possibilities for vision care worldwide.
In addition to establishing the professorship, Dr. Munsen is also supporting a scholarship at St. Olaf College, his alma mater, for underserved students, underscoring his generous spirit and broad philanthropic vision. Whether advancing medical care, mentoring future physicians, or expanding access to education, Dr. Munsen is deeply committed to giving back and making a lasting difference in the lives of others.
To donate to the Richard S. Munsen, M.D. Professorship in Ophthalmology, visit - Richard S Munsen Fund.

InSight Newsletter Winter 2025
InSight Newsletter Winter 2025
Message from the Chair
Welcome to the Winter 2025 edition of the Department of Ophthalmology InSight Newsletter.
This issue's research spotlight shines on the groundbreaking research of faculty members Drs. Debarshi Mustafi and Andrew Stacey. They have developed a novel blood test for children with retinoblastoma, a rare, hereditary eye cancer, that can tell which parent’s DNA carried the disease-causing RB1 gene mutation. The new test likely will have applications for other genetic diseases in which parent-of-origin influences patients’ risk.
We also highlight the newest research faculty member, Yuzuru Sasamoto, MD, PhD, who studies cornea regeneration. We are fortunate to have him joining our Vision Science Center at South Lake Union.
Our patient care spotlight features the trauma and consult service at Harborview Medical Center under the direction of Clinical Associate Professor Jennifer Yu, MD, PhD. Our department handles about 1,500 emergency room visits a year. It is one of the few ERs to have dedicated ophthalmology space within the ER.
In Education, we are pleased to share the results of our fellowship and residency program matches for 2025-26, as we welcome five incoming residents and five fellows, including our new glaucoma fellowship.
Finally, in our philanthropy spotlight, longtime department supporters Jack and Pam Jolley have established a unique funding initiative designed to provide immediate financial support to early-stage research. This strategic approach to funding is poised to make a lasting impact, providing researchers like Assistant Professor Chris Fortenbach, MD, PhD, the inaugural fellowship holder, with the resources needed to advance innovations in ophthalmology.
For more news and updates, please visit our website at ophthalmology.washington.edu and our Facebook, Instagram, and LinkedIn pages.
Russell N. Van Gelder, MD, PhD,
Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Director, Roger and Angie Karalis Johnson Retina Center
Director, Vision Science Center
Research: Drs. Mustafi and Stacey develop a test to detect parent-of-origin in hereditary eye cancer
UW ophthalmology faculty and Roger and Angie Karalis Johnson faculty who care for children with retinoblastoma, a rare, hereditary eye cancer, have developed a novel blood test that can tell which parent’s DNA carried the disease-causing RB1 gene mutation.
That distinction is meaningful because male and female copies of the mutation are associated with different disease trajectories, the researchers found, and likely would influence doctors’ treatment recommendations.
“Depending on which copy you have, that could reflect the cancer’s severity and its likely response to chemotherapy,” said Dr. Debarshi Mustafi, a UW assistant professor of ophthalmology and Karalis Johnson Center researcher.
The new gene-sequencing technique that powers the blood test can also detect parent-of-origin even when the child carries a de novo variant, one that arises spontaneously and is not present in either parent. These de novo cases are the predominant cause of all cancers and account for 90% of all inherited cases of retinoblastoma.
The findings were published Dec. 26 in the journal JCI Insight. The co-lead authors were Mustafi and Dr. Andrew Stacey, UW associate professor of ophthalmology and director of ocular oncology.
Retinoblastoma is rare, affecting about 200 to 300 children annually in the United States. The condition disrupts the normal development of the retina, the light-sensitive tissue in the back of the eye. Starting during fetal development, these cancerous cells proliferate out of control and form tumors.
Children in developed countries are diagnosed by age 2, on average, Mustafi said. Often, an early hint of the disease is a pupillary discoloration seen in a photo of the child or an eye that has trouble tracking.
Without treatment, retinoblastoma can spread through the optic nerve into the brain. Even when tumors are ablated with radiation or treated with chemotherapy, related metastases can emerge years later in distant organs.
“If we can catch the tumor early, we can save the eye — and what we found in this study is that your parent-of-origin makes a difference here: When mutations came from the maternal copy, patients’ eyes were saved more often,” Mustafi said. “If they got it from the paternal DNA, we are less likely able to save the eye. Our preliminary data also shows that a secondary cancer such as sarcoma is more likely with the paternal mutation.”
Awareness of parental disease origin, he added, could influence doctors to recommend aggressive therapies earlier in a child’s course of care or to take more, or fewer, steps to save an affected eye.
“We could counsel a family that, instead of going for these heroic measures, they may be better off taking the eye out and preventing the spread,” Mustafi said. “Our finding will not only inform how we treat a child in the beginning, but how we screen them for their entire life. We think this will have a huge impact on surveillance of cancer patients.”
Creating the novel genetic test
The researchers didn’t set out to create a novel genetic test for retinoblastoma. Mustafi described a 2023 conversation in which Stacey expressed frustration with the wait — typically one to six months — to get a commercial lab’s confirmation of whether a child has the RB1 mutation.
“Our initial goal was to see if we could confirm the diagnosis faster. I told him that my lab was working on a method that could get him an answer in a day or two,” Mustafi said.
His lab scientists ended up devising a gene-sequencing technique that simultaneously identifies not only the RB1 mutation but also other DNA-based modifications.
“Two things happen with DNA: One is a mutation, in which some of your normal genetic code is switched out for other code. Your DNA is changed. But another thing that happens, called methylation, is a kind of modification signal that is switched on or off,” Mustafi said.
“With RB1, we saw that Dad’s copy of the modification signal is distinct from Mom’s,” he added. “So, when we put the mutation together with the modification signal, we were able to tell from the child’s blood whether they got the mother’s or the father’s chromosomal copy — and without having to test either parent.”
They also met their goal of a 24-hour turnaround for diagnostic results.
The experimental gene-sequencing technique’s accuracy was validated with blood samples from 16 pediatric patients at Seattle Children’s. Seven had familial-origin cases and nine had de novo disease.
“The ability to assign parent-of-origin in all cases of retinoblastoma showed that harboring disease-causing variants on the paternally inherited allele, whether arising familial or de novo, is associated with more advanced cancer staging at presentation and significantly greater risk of chemotherapy failure,” the study authors wrote.
The new test likely will have applications for other genetic diseases in which parent-of-origin influences patients’ risk, Mustafi suggested. First, though, the researchers will measure its predictive accuracy in a larger group of patients.
“We are partnering on a clinical trial with other large institutions that see a lot of retinoblastoma, like St. Jude's Research Hospital (Memphis), MD Anderson (Houston) and Children's Hospital (Los Angeles),” he said.
To support this research, visit https://give.uwmedicine.org/give/?source=OOSFND
Research: Meet Yuzuru Sasamoto, MD, PhD, new research faculty member
Yuzuru Sasamoto, MD. PhD has joined the faculty as an acting assistant professor and will have a lab in the Vision Science Center at South Lake Union.
Dr. Sasamoto studies corneal regeneration using techniques such as direct reprogramming, induced pluripotent stem cells (iPSCs), and limbal progenitor cells.
He is currently working on the comprehensive characterization of ocular surface epithelium from conjunctiva to cornea. Ultimately, the lab’s focus is on the discovery of new therapies that could benefit those who are affected by corneal disease.
Born and raised in Osaka, Japan, Dr. Sasamoto received his MD from Osaka University Medical School in Japan. After completing his medical training in ophthalmology, he received a PhD from Osaka University Graduate School of Medicine in 2016. He joined the Frank lab at Harvard in 2016 and opened his NIH-funded lab at Boston University in 2022. His wife, Naoko, is an epidemiologist doing ovarian cancer research at Fred Hutch Cancer Center, and they have three children. In his free time, he enjoys table tennis.
Patient Care: Trauma and Consult Service
Tucked away in a hallway behind the busy emergency room and trauma center at Harborview Medical Center is a small exam room dedicated to urgent ophthalmology cases.
The Department of Ophthalmology handles about 1,500 emergency room visits a year. It is one of the few ERs to have dedicated ophthalmology space within the ER.
“We are delighted to have this space. We used to haul the equipment around the emergency department or bring patients to the clinic,” said Dr. Jennifer Yu, MD, PhD, Clinical Associate Professor and director of the Trauma and Consult Service at Harborview and the 4-West Ophthalmology Clinic.
The ER exam room was recently upgraded with a new ultrasound device, a YAG laser, and a combined fundus camera/OCT machine with robotic capability.
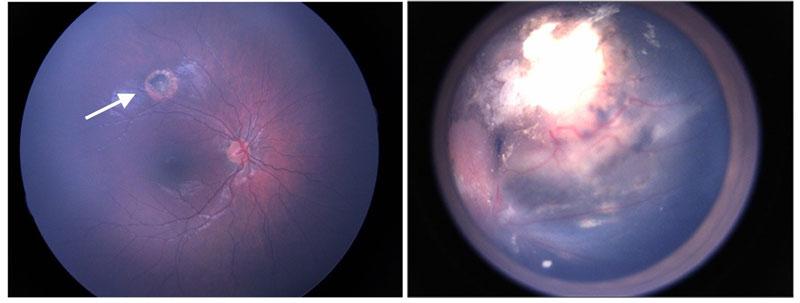
Patients are triaged through the ER and sent to ophthalmology for a variety of concerns. These include traumatic globe injuries, lacerations to the eyelid, removal of foreign bodies in the cornea, infections, and retinal detachments.
“We see pretty much everything in this room,” Dr. Yu said. “The volumes have grown each year.”
Often, the patients are referred to the Harborview ER from community physicians or hospitals that may not have an ophthalmology service. Furthermore, Harborview is the region's only level 1 trauma center, handling the most severe trauma cases in a five-state area.
During the day, a resident consults with emergency patients and those in the hospital. After hours, the on-call resident handles emergencies.
“They typically see between three and eight patients daily through the ER. They also go see patients on the floor, as most of them aren’t able to go to clinic for their examination, so we go to them with our portable equipment,” Dr. Yu said. “There can be as many as 10-13 inpatient checks each day, and many of them need to be seen repeatedly during their hospital stay.’
Marcus Turner, MD, a second-year resident, recently completed his five-week rotation as the consult resident.
“This is a busy level 1 trauma center, and the sheer volume of what I see, doing procedures, managing complex cases, working with different attending physicians, has been a tremendous learning experience for me,” Dr. Turner said.
Dr. Yu said patients who come through the ophthalmology ER are stabilized and hospitalized if needed. Many are referred to 4-West, the Harborview ophthalmology clinic, and the Eye Institute for follow-up care.
“Often the patients we see don’t have anywhere else to go,” Dr. Yu said. “The culture at Harborview is to support that patient. It's a gratifying part of being here.”

Remembering Avery Weiss, MD
Avery Weiss, MD, Professor Emeritus of Ophthalmology, passed away from brain cancer on Dec. 1, 2024. He was 75. Dr. Weiss joined UW Department of Ophthalmology in 1991. For many years, he was the sole pediatric ophthalmologist, and served for many years as Ophthalmology Division Chief at Seattle Children’s Hospital. He was a fixture at the hospital and an important member of multidisciplinary teams that diagnosed complex patients.
“Avery threw himself into his research and was even writing papers in his final weeks,” said Russ Van Gelder MD PhD, Bucey Chair of the Department of Ophthalmology. “He was an important inspiration for many students and trainees to enter ophthalmology and pediatric ophthalmology careers. Avery will be deeply missed.”
Dr. Weiss earned his M.D. at the University of Miami, followed by residency and fellowships at Barnes Jewish Hospital in St. Louis. He served on the editorial board of EyeNet, the official journal of the American Academy of Ophthalmology. He published over 100 papers and book chapters and was a reviewer for 18 journals.

Education: New fellow and residents matched with UW Ophthalmology
Match Day for fellowships was held in December and the following have matched with the UW Department of Ophthalmology:
Retina (two years)
Alexander Tseng, MD, PhD
Residency: USC / LA General Medical Center
Glaucoma (new fellowship for 2025-26)
Brian Nguyen, DO
Residency: Corewell Health (Taylor) Ophthalmology
Uveitis
Fatma Dihowm, MBBCh, MS
Residency: Misurata Medical Center, Libya
Pediatrics
Catherine Culp, MD
Residency: George Washington University
Oculoplastics (two years)
Ryan Gabbard, MD
Residency: University of South Carolina
Three of our current fourth-year residents are matched for fellowships elsewhere:
Sam Kushner-Lenhoff, MD—Retina, UC Davis
Nicole Mattson, MD—Glaucoma, University of Iowa
Ryan Yanigahara, MD—Medical Retina, Retina Consultants of Texas
Welcome to the Residency Class of 2029!
InSight Newsletter Fall 2024
Fall 2024
Message from the Chair, Russ Van Gelder, MD, PhD
Welcome to the Fall 2024 edition of the Department of Ophthalmology InSight Newsletter. This year has marked many notable anniversaries – 60 years as a department of the UW School of Medicine, 15 years for the Eye Institute, our 15th Gained in Translation research symposium, and the 5th anniversary of the Karalis Johnson Retina Center.

Featured in this issue, we held a celebration and reunion for the Community Action Board on Oct. 14, honoring those who have served and continue to serve as ambassadors and supporters of our department. Learn more about the CAB here.
Gained in Translation, the annual symposium of ophthalmology clinicians and researchers from UW, Oregon Health Sciences University, and the University of British Columbia, was held on Nov. 2, with our department hosting on the South Lake Union campus. Read more about this year’s conference in this issue.
This issue's research spotlight shines on retinal specialist Assistant Professor Chris Fortenbach’s work investigating the therapeutic potential of photoswitches to restore vision in degenerated retinas in his lab at the Vision Science Center in South Lake Union.
In our patient care feature, we highlight the newest faculty member, Assistant Professor Minh Nguyen, MD, a graduate of our residency program. We were so fortunate to welcome him back to the department in August.
Finally, in our philanthropy spotlight, The Violet Sees Fund for Pediatric Ophthalmology Research has provided crucial support to Dr. Michelle Cabrera, professor and director of pediatric ophthalmology, and Dr. Andrew Stacey, associate professor and director of ocular oncology, over the past five years, enabling them to expand their research and improve patient care. Thanks to Violet’s family for their generous support of our department.
Please visit our website at ophthalmology.washington.edu and our Facebook, Instagram and LinkedIn pages for more news and updates.
Russell N. Van Gelder, MD, PhD,
Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Director, Roger and Angie Karalis Johnson Retina Center
Director, Vision Science Center
Research Spotlight: Fortenbach Lab investigating the therapeutic potential for photoswitches to restore vision
Age-related macular degeneration and retinitis pigmentosa are degenerative diseases affecting millions of people worldwide. They cause progressive loss of the outer retina, characterized by the death of rod and cone photoreceptors. This leads to declining
vision and, in some cases, blindness. While treatments to prevent degeneration remain under investigation, therapies to restore vision have begun to emerge, including synthetic small molecules known as photoswitches.
Assistant Professor Chris Fortenbach, MD, PhD, is investigating the therapeutic potential for photoswitches to restore vision in degenerated retinas in his lab at the Vision Science Center in South Lake Union. These light-sensitive small molecules bind to the degenerating retina and confer new light sensitivity to retinal cells. Several generations of these molecules have been developed with differing cell target specificity and sensitivity.
In contrast to other therapies requiring surgery, photoswitches can be delivered via intravitreal injection, a procedure performed over 20 million times per year globally. Most recently, promising phase 1 clinical trial data have demonstrated vision restoration in several human subjects.
The Fortenbach Lab is researching the mechanisms by which photoswitches restore light sensitivity and methods to improve visual outcomes among treated individuals. The lab uses a combination of electrophysiology methods, including whole-cell and multielectrode array recordings, in conjunction with machine learning to assess the ability of photoswitches to encode visual information. Overall, the lab's goal is to help develop a medication capable of restoring sight and improving the quality of life for patients with vision loss.
Dr. Fortenbach joined the faculty in August 2023 after completing his ophthalmology residency and vitreoretinal surgery fellowship at the University of Iowa Hospitals and Clinics. His clinical practice is at the Karalis Johnson Retina Center and the Veterans Affairs Puget Sound Healthcare System.
Dr. Fortenbach grew up in Northern California, where he attended the University of California, Davis for his undergraduate education. He stayed on for the MD/PhD program, where he earned his PhD in Biochemistry, Molecular, Cellular, and Developmental Biology, studying how retinal neurons convey the presence of light.
He first became involved in research in high school and joined a plant pathology lab at UC Davis during his undergrad years studying food science. He became interested in medicine while working in a clinic serving the underserved. Joining the MD/PhD program, he gained his first experience in vision science.
“Vision science is unique in that we can trace it from basic scientific principles to human perception,” Dr. Fortenbach said. “This understanding means that when things go awry, we have a solid foundation in science from which to build new treatments of ophthalmic disease.”
Dr. Fortenbach and his wife, Jennie, a pediatric physical therapist, are the parents of a two-year-old girl and are expecting their second child. In his spare time, Dr. Fortenbach enjoys backpacking, cycling, tennis, and cooking.
Flagship AI-ready dataset released in type 2 diabetes study
UW Ophthalmology researchers Dr. Aaron Lee and Dr. Cecilia Lee are releasing the flagship dataset from an ambitious study of biomarkers and environmental factors that might influence the development of type 2 diabetes. Because the study participants include people with no diabetes and others with various stages of the condition, the early findings hint at a tapestry of information distinct from previous research.
For instance, data from a customized environmental sensor in participants’ homes show a clear association between disease state and exposure to tiny particulates of pollution. The collected data also includes survey responses, depression scales, eye-imaging scans and traditional measures of glucose and other biologic variables.
All of these data are intended to be mined by artificial intelligence for novel insights about risks, preventive measures, and pathways between disease and health.
“We see data supporting heterogeneity among type 2 diabetes patients — that people aren’t all dealing with the same thing. And because we’re getting such large, granular datasets, researchers will be able to explore this deeply,” said Dr. Cecilia Lee, Klorfine Family Endowed Chair and UW professor of ophthalmology.
She expressed excitement at the quality of the collected data, which represent 1,067 people, just 25% of the study’s total expected enrollees.
Lee is program director of AI-READI (Artificial Intelligence Ready and Equitable Atlas for Diabetes Insights). The National Institutes of Health-supported initiative aims to collect and share AI-ready data for scientists worldwide to analyze for new clues about health and disease.
The initial data release is highlighted in a paper published in the journal Nature Metabolism. The authors restated their aim to gather health information from a more racially and ethnically diverse population than has been measured previously, and to make the resulting data ready, technically and ethically, for AI mining.
“This process of discovery has been invigorating,” said Dr. Aaron Lee, Dan and Irene Hunter Endowed Professor of ophthalmology and the project’s principal investigator. “We’re a consortium of seven institutions and multidisciplinary teams that had not worked together before. But we have shared goals of drawing on unbiased data and protecting the security of that data as we make it accessible to colleagues everywhere.”
At study sites in Seattle, San Diego, and Birmingham, Alabama, recruiters are collectively enrolling 4,000 participants, with inclusion criteria promoting balance:
- race/ethnicity (1,000 each – white, Black, Hispanic and Asian)
- disease severity (1,000 each – no diabetes, prediabetes, medication/non-insulin-controlled and insulin-controlled type 2 diabetes)
- sex (equal male/female split)
“Conventionally scientists are examining pathogenesis — how people become diseased — and risk factors,” Aaron Lee said. “We want our datasets to also be studied for salutogenesis, or factors that contribute to health. So if your diabetes gets better, what factors might be contributing to that? We expect that the flagship dataset will lead to novel discoveries about type 2 diabetes in both of these ways.”
By collecting more deeply characterizing data from a lot of people, he added, the researchers hope to create pseudo health histories of how a person might progress from disease to full health and from full health to disease.
Hosted on a custom online platform, the data are produced in two sets: a controlled-access set requiring a usage agreement, and a registered, publicly available version stripped of participants' HIPAA-protected information.
The pilot data release (summer 2024) involving 204 participants has been downloaded by more than 110 research organizations worldwide. Researchers must verify their identity and agree to ethical-usage terms. (Learn more about accessing the data at aireadi.org.)
The AI-READI Consortium comprises the University of Washington School of Medicine, University of Alabama at Birmingham, University of California San Diego, California Medical Innovations Institute, Johns Hopkins University, Native Biodata Consortium, Stanford University and Oregon Health & Science University.
The project is based at the Angie Karalis Johnson Retina Center at UW Medicine in Seattle.
This work was supported by the NIH (grants OT2OD032644 and P30 DK035816). The authors’ conflict-of-interest statements are in the published paper, which will be provided upon request.

Patient Care Spotlight: Dr. Minh Nguyen
Dr. Minh Nguyen joined the faculty as an assistant professor on Aug. 1, but he is familiar with the department. He completed his ophthalmology residency at UW in 2022. He returned to UW after completing a fellowship in cornea, external disease, and refractive surgery at the world-renowned University of California, San Francisco/ F.I. Proctor Foundation.
Born in Vietnam, he came to the U.S. at age 19 in 2007. He attended community college to become proficient in English before enrolling at UCLA, receiving a Bachelor of Science in Molecular, Cell, and Developmental Biology.
“It was disorienting at first, coming from Vietnam alone,” Nguyen said. “I went to community college in Cupertino and lived with a host family. It’s funny, but I really learned English from reading Harry Potter and watching Grey’s Anatomy.”
After graduating from college, he worked in a lab for two years and thought he might become a pediatrician. Breaking out of his comfort zone in LA, he accepted a full scholarship to medical school at the University of Wisconsin, Madison.
“I had done cutting-edge research on epigenetics at UCLA, and I was fortunate to continue this work in medical school using CRISPR-Cas9 to generate retinal cells from induced pluripotent stem cells. These experiences and the awesome mentorship at UW Madison got me interested in ophthalmology,” he said.
He visited the Seattle VA as a medical student in Wisconsin and was impressed. He was matched into the UW residency program in 2019.
Then, the COVID-19 pandemic happened, and the residents were on the front lines.
“We had such an awesome class of 2022,” he said. “It was a very uncertain time, and we supported and pushed one another.”
In residency, he learned he liked to do corneal transplants and ocular infectious disease, so he went to UCSF/Proctor Foundation to complete a fellowship in cornea, external disease and refractive surgery.
After fellowship, he practiced at Kaiser Permanente in Southern California for a year before accepting the position at UW.
Dr. Nguyen’s approach to patient care is grounded in treating each individual as a cherished member of his own family, not merely as a case of illness. He is committed to their holistic well-being, addressing not only their eye health but also their mental and emotional needs.
Dr. Nguyen and his wife, Chau, have two children. In his free time, Dr. Nguyen enjoys hiking and mushroom hunting with his family and delights in exploring tidepools at the beach.
Gained in Translation brings together clinicians and vision scientists from UW, UBC, and OHSU
The 15th Annual Gained in Translation Symposium was held on Nov. 2 at UW Medicine South Lake Union in Seattle. This symposium brings together clinicians and vision scientists from the University of Washington, the University of British Columbia, and Oregon Health Sciences University. The event rotates between the sites each year.
Presentations focused on bridging the gap between disease treatment and the latest translational and basic research advances. Areas of synergy are identified for future collaboration between these institutions.
Sue Brockerhoff, PhD, UW Professor of Biochemistry and Adjunct Professor of Ophthalmology, was honored with the Helen Keller Award at the event. The Lions Clubs serving Washington and British Columbia give the award annually to honor an individual at the host institution who has made significant contributions to vision science or ophthalmology care.
Dr. Brockerhoff's overall research goal is to understand the biology of the cone photoreceptor and apply this knowledge to dissect the molecular basis of human retinal disease.
Speakers on vision research from the UW Department of Ophthalmology included Ricky Wang, PhD, George and Martina Kren Endowed Chair in Ophthalmology Research; Professor of Bioengineering and Ophthalmology; Chris Fortenbach, MD, PhD, Assistant Professor of Ophthalmology, and Ram Sabesan, PhD, Kren Professor of Ophthalmology.
The keynote speaker was Marco A. Zarbin, MD, PhD, who has been Chair of the Institute of Ophthalmology and Visual Science at Rutgers-New Jersey Medical School for nearly 30 years. Dr. Zarbin specializes in vitreoretinal surgery and research.

Seattle Family’s Mission: From Violet’s Blindness to Global Action on Preventable Blindness
Around the world, a child loses their sight every minute, and 80 percent of these cases are preventable or treatable. It’s a staggering reality, but for many children, the battle for sight can be won—if they have access to the proper care.
One local family knows this all too well. The saying, “A winnable battle should never be lost,” resonates deeply with them, especially regarding their daughter and granddaughter, Violet. Born completely blind, Violet was diagnosed with total bilateral congenital cataracts. Her lenses, which should have been clear, were instead completely clouded.
Fortunately, because the family lives in a place with advanced medical care and the means to access it, Violet was diagnosed at just 10 weeks old. She had her first surgery a week later—before too much irreversible damage could occur. Violet’s journey could have been very different without the timely intervention, and her family knows how fortunate they are.
There are families, both around the world and here in America, just like Violet’s, who lack the medical infrastructure and resources to diagnose, treat, and rehabilitate their children in time. Many of these children could have the gift of sight if only they had access to proper care. That’s why Violet's family started Violet Sees—an organization dedicated to preventing childhood blindness and ensuring families get the needed help.
Violet Sees covers the cost of glasses to children, ensuring that even basic vision impairments don’t hinder a child’s future.
The organization also works to expand and improve vision screening programs so more children can be screened as early as possible—crucial for preventing long-term damage. Additionally, it funds research to find the best treatments for childhood vision conditions, ensuring more children can receive life-changing care.
The Violet Sees Fund for Pediatric Ophthalmology Research has provided crucial support to Dr. Michelle Cabrera, professor and director of pediatric ophthalmology, and Dr. Andrew Stacey, associate professor and director of ocular oncology, over the past five years, enabling them to expand their research and improve patient care.
In the Cabrera lab, the fund has been instrumental in advancing the development of a non-contact eye imaging device for premature newborns. This handheld device uses cutting-edge technology to scan a newborn’s eyes without physical contact, eliminating the need for additional medications or eye drops. The device employs optical coherence tomography (OCT), a technology that uses light waves to capture high-resolution cross-sectional images of the retina. Dr. Cabrera’s research analyzes these OCT images to identify key features and patterns that can predict the risk of blindness from Retinopathy of Prematurity (ROP), a leading cause of vision loss in premature infants.
For Dr. Stacey, support from the Violet Sees Fund has enabled groundbreaking research on retinoblastoma, a rare but serious eye cancer in children. This hereditary disease develops from cell mutations in the retina, and the funding is fueling efforts to develop a gene therapy approach that aims to stop these mutations before tumors can form—potentially halting retinoblastoma in its tracks. The funding also supports advancements in early detection, a critical factor in improving outcomes for children affected by this devastating condition.
The work of Violet Sees is a testament to the power of hope, determination, and the belief that every child deserves the chance to see the world around them. Violet’s journey from blindness to sight reminds us that access to timely medical care can make all the difference, but for many families around the world, this access is still out of reach.
For more information on Violet Sees, visit violetsees.org.
To support this fund, visit give.uwmedicine.org/ Violet Sees Fund for Pediatric Ophthalmology Research.

Community Action Board celebrates its 15th anniversary
The Department of Ophthalmology celebrated the Community Action Board's 15th anniversary at a dinner on Oct. 14 at the Women’s University Club.
The Community Action Board is a group of committed volunteers who advance the Eye Institute’s mission by serving as ambassadors in our community, advising faculty on matters of strategic importance, and generously supporting our mission. Philanthropic gifts help to accelerate innovation in the form of seed grants for our faculty research. We are honored and privileged to work with such a fine group of individuals as we pursue our mission of eliminating blinding eye disease.
The CAB was formed after the Eye Institute opened in 2009, and more than 50 people have served.
The Community Action Board has provided support in many areas, including
- Art for the Institute
- Community outreach for talks and support
- Educational materials for our students and residents
- Outreach videos for the institute
- Support for students and trainees in our laboratories and clinics
- Latham Vision Research Innovation Awards
- Lions Gift of Sight
- Johnstone and Freeman Resident Travel Awards
- Medical Student Interest Night hosting
The holders of 13 endowed faculty positions were honored at the dinner, including two new faculty fellowships. Ethan Buhr, PhD, research associate professor, has been appointed to the Ragen Family Faculty Fellowship, and Chris Fortenbach, MD, PhD, assistant professor, to the Jolley Faculty Fellowship.
Since opening in 2009, the Eye Institute has seen more than 500,000 patient visits and 70,000 individual patients. Eye Institute faculty have performed over 40,000 surgeries and provided millions of dollars of charity care. The department’s endowment has grown to nearly $50 million, and the department now ranks third in the nation for research funding from the NIH.

InSight Newsletter Summer 2024
Summer 2024
Message from the Chair, Russ Van Gelder, MD, PhD
Welcome to the Summer 2024 edition of the Department of Ophthalmology InSight Newsletter. In this issue, we welcome our new residents and fellows, who joined us in July. Our residency program continues to be one of the most competitive in the country. Our strong fellowship programs in retina, oculoplastics, uveitis, and pediatrics will expand with new programs in glaucoma and neuro-ophthalmology in 2025-26.
The research spotlight in this issue shines on two recent impactful projects by our faculty.

The first is Professor and Klorfine Family Endowed Chair Dr. Cecilia Lee’s work summarized in a recently published paper in the Journal of Alzheimer’s Disease, which details progress to detecting Alzheimer’s disease early with home testing of retinal changes linked to dementia. Dr. Lee and her colleagues previously found a significant link between dementia and age-related macular degeneration, diabetic retinopathy, and glaucoma.
The second is a grant awarded to Assistant Professor Dr. Debarshi Mustafi and Adjunct Associate Professor Dr. Tim Cherry of Seattle Children’s from Seattle Children’s Research Institute to determine the genetic causes of unsolved inherited retinal diseases (IRD). Leveraging clinical expertise and research capabilities, the collaborative effort of Drs. Cherry and Mustafi seek to unlock insights into IRDs and explore gene editing therapeutic strategies.
In our patient care feature, we highlight our ocular oncology service led by Associate Professor Dr. Andrew Stacey. Our department is fortunate to have the expertise of Dr. Stacey, the only full-time ocular oncologist in the WWAMI region (Washington, Wyoming, Alaska, Montana, and Idaho). His service manages all types of ocular tumors from conjunctiva to choroid.
In our education spotlight, learn about our clerkship program for medical students, which is led by Assistant Professor Dr. Shu Feng. The clerkship gives medical students an introduction to ophthalmology and our residency program.
Finally, in our philanthropy spotlight, we were honored to present the Roger Johnson Award for Macular Degeneration Research to Dr. Raj Apte of Washington University in St. Louis at the 50th Resident Alumni Day on June 15. Learn more about the award created with a generous gift from Roger and Angie Karalis Johnson and Dr. Apte’s research.
On behalf of the department, thank you for your continuing support of our mission to alleviate suffering from eye disease. Please visit our website at ophthalmology.washington.edu and our new Facebook and Instagram pages for more news and updates.
Russell N. Van Gelder, MD, PhD,
Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Director, Roger and Angie Karalis Johnson Retina Center
Director, Vision Science Center
Research Spotlight:
Alzheimer's vision study improved with home tests
There is conflicting research on the strength of relationships between retinal biomarkers and Alzheimer’s disease and related dementias. Limited sample sizes, study designs and protocol differences have led to mixed results in exploring whether features on the back of the eye are associated with development of dementia.

A new paper suggests that by adding a home testing element to their research, Department of Ophthalmology Professor and Klorfine Family Endowed Chair Dr. Cecilia Lee and her colleagues from the University of Washington School of Medicine and the Kaiser Permanente Washington Health Research Institute have ironed out a difficult wrinkle.
The group believes their study results will move them closer to a reliable way to detect Alzheimer’s disease early. Their paper, published June 25 in the Journal of Alzheimer’s Disease, details progress on the project.
“We know that just looking at the diagnosis of eye diseases can tell us that somebody's at increased risk of Alzheimer's disease,” said Lee. “Now we can do so much better with characterizing the eye, particularly the retina, the neural tissue of the eyeball, because we have all these noninvasive techniques. We can measure visual function and characterize microscopic features of the retina.”
Lee’s Eye ACT study recruited 330 participants from within the ongoing Adult Changes in Thought study whose retinas are imaged every two years. About a third can’t come to the clinic for evaluation and need home testing. Since Alzheimer’s is so difficult and expensive to diagnose, the hope is by tracking retinal changes over time, researchers can use artificial intelligence to correlate those changes with the development of dementia and understand at what point these retinal changes occur before or while cognition becomes impaired.
One hitch, however, has been the lack of testing techniques outside of clinic settings. This has meant that potential research participants who could not get to a clinic were left out of the data. These people are often older and have more complex health conditions. Not including them as participants was a potential flaw in study design.
This research was funded in 2019 with a $17.2 million grant from the National Institute on Aging. The grant came after Lee and colleagues published a 2018 study that found a significant link between dementia and age-related macular degeneration, diabetic retinopathy and glaucoma.
The team also found that cataract surgery was associated with a 30% lower risk of dementia in a subsequent study. She hopes the NIA will extend the grant another five years this year so they better understand these results and discover more in this unique population.
“If you ask me about a result, I promise you that I can find a paper that reports a conflicting outcome,” Lee said. “There are a lot of controversies about, say, what part of the retina is associated with Alzheimer's? Is it really Alzheimer's? Or is it any neurodegenerative conditions like Parkinson’s disease, vascular dementia, frontotemporal dementia, and so on? Is it really age-related? Where do you need to look?”
Dr. George Perry, the editor-in-chief of the Journal of Alzheimer’s Disease, agrees and has identified Lee’s work as of particular interest “as the eye changes have been somewhat controversial and this work clarifies.”
Lee and team have been using data gathered from participants in the Adult Changes in Thought study established in 1994 as a collaboration between Kaiser Permanente Washington Health Research Institute and UW School of Medicine. ACT is a living laboratory of aging and the brain that includes health information about Kaiser Permanente Washington participants 65 and over.
The grants have supported continuous regular collection of extensive data for Alzheimer’s disease research and brain aging among others. The ACT information is especially valuable, Lee said, because it is community based, not just highly selected samples from referral clinics. All patients are likely getting the same kind and level of comprehensive medical care as they age.
The study’s investigative team includes expertise in Alzheimer’s disease and related dementia, neuropsychology, neuroimaging, ophthalmic imaging, big data and artificial intelligence. Lee believes the work they’ve done to date has laid the groundwork for moving past the so-far muddled results in this area of study.
“We are already seeing significant results just from looking at the first 330, and then now those people are coming back to follow up,” Lee said. “We are so grateful to our Eye ACT and ACT participants. The study will continue to generate more results and this is what we need.”
This research was funded by the National Institute on Aging (R01AG060942, U19AG066567, U01AG006781). Additional funding included NIH grant OT2OD032644, the Latham Vision Research Innovation Award, the Klorfine Family Endowed Chair, the Karalis Johnson Retina Center and an unrestricted grant from Research to Prevent Blindness.
Research to study the genetic causes of inherited retinal diseases
Inherited retinal diseases (IRDs) affect one in 3,000 people, and almost one-third of cases will have inconclusive genetic testing, which limits therapeutic opportunities that may restore sight. The precise identification of genotypic causes of IRDs has taken on new importance as treatment is only indicated for specific genetic defects, especially with the emergence of retinal stem-cell-based therapies.
Tim Cherry, PhD, Associate Professor in the Department of Pediatrics and Adjunct Assistant Professor of Ophthalmology. and Debarshi Mustafi, MD, PhD, Assistant Professor in the Department of Ophthalmology, were awarded a $150,000 Clinical & Research Synergy Pilot Award from Seattle Children’s Research Institute to determine the genetic causes of unsolved IRDs and address this important issue.
Dr. Mustafi is a pediatric retina specialist at Seattle Children’s Hospital and, in connection with the genetics department, has a focused clinic to help identify IRD patients to coordinate their phenotypic workup and genetic testing. Although a large percentage of patients received a causative diagnosis, many families were left with inconclusive results, especially when there were findings of variants of uncertain significance that would require further research into their possible pathogenicity.
To help provide further disease insight and develop gene-editing techniques to correct these changes in patient cells, Dr. Mustafi partnered with Dr. Cherry. The Cherry Lab investigates how the visual system develops and how genetic variations contribute to blindness and other visual disorders. Dr. Mustafi will lead the clinical portion of this project, whereas Dr. Cherry will lead the project's research component.
The investigators intend to enhance the IRDs using patient-derived retinal organoids. By investigating genetic causes, mechanistic features, and therapeutic targets, they will seek to address the challenges patients face with inconclusive genetic testing results. Leveraging clinical expertise and research capabilities, the collaborative effort of Drs. Cherry and Mustafi seek to unlock insights into IRDs and explore gene editing therapeutic strategies.

Patient Care Spotlight: Ocular Oncology
Ocular oncology is a specialty within ophthalmology that deals with diagnosing and treating tumors on the surface and inside of the eye. Eye cancer can affect any structure in the eye and can be challenging to diagnose.
The Department of Ophthalmology is fortunate to have the expertise of Associate Professor Andrew Stacey, MD. He runs the only full-service ocular oncology unit in the WWAMI region (Washington, Wyoming, Alaska, Montana, and Idaho). He sees patients at the UW Medicine Eye Institute at Harborview and the Ophthalmology Clinic at Seattle Children’s.
After the tumor is diagnosed, treating it often requires a team from many medical specialties outside of Ophthalmology. Dr. Stacey teams with pediatricians, medical oncologists, radiation oncologists, and interventional radiologists at UW, Fred Hutch, and Seattle Children’s.
“There are two main options when treating eye cancers such as ocular melanoma,” Dr. Stacey said. “One is a surgical option, and the other is radiation. We have all modalities available at UW. For many patients, proton beam radiotherapy is used. It is a focused radiation beam that can treat the cancer precisely and limiting damage to the surrounding ocular structures.”
In 2015, the University of Washington created a first-of-its-kind proton beam and has now treated 400 patients. “Our innovations at UW have allowed modern proton beams to be applied to ocular tumors,” he said.
Learn more about proton therapy for eye cancer in this video.
Dr. Stacey has developed a highly collaborative network of eye cancer specialists worldwide who share information and expertise to benefit patients.
Working with Ophthalmology faculty colleagues Professors Aaron and Cecilia Lee, Dr. Stacey is using AI to create an open-source, international eye cancer image library that makes that data accessible to researchers. Currently, 15 sites from four countries are enrolled, with over 3,000 images from 857 unique melanomas.
“We are just at the beginning, but the power of collaborative databases is real,” Dr. Stacey says.
Stacey’s effort includes creating an international network to bridge the global disparities in treatment for retinoblastoma, an eye cancer that affects children and often goes untreated in lower-income areas. Stacey and his colleagues worldwide have demonstrated the global disparity in outcomes of children with retinoblastoma for the first time. They have shown that children from low-income countries present to the hospital later and have worse outcomes than children from higher-income countries. Their research has also led to numerous publications on topics such as the effect of national income on the lag time between the onset of signs and symptoms and referral to a retinoblastoma center, the global gender disparity in the diagnosis of retinoblastoma, and elucidating factors that lead to families abandoning care for children with retinoblastoma.
Locally, Dr. Stacey and colleagues in the Department of Ophthalmology and the School of Medicine are working on improving diagnostics and therapeutics for retinoblastoma, developing non-invasive maternal testing for the disease, and gene-based treatments.
Dr. Stacey joined the faculty in 2016. He grew up in Northeast Ohio and earned a bachelor’s and master's degree in statistics at Brigham Young University, where he was also a linebacker on the football team. During college, he took two years off school and athletics to volunteer for his church in northern Italy.
He earned his medical degree from Ohio State University and completed his ophthalmology residency at the University of Michigan Kellogg Eye Center. He then completed a fellowship in ocular oncology at Moorfields Eye Hospital in London, U.K.
Dr. Stacey lives in Seattle with his wife and four children. In his free time, he enjoys running, mountain biking, fly fishing, volunteering at his church, and being in the mountains with his family.

Nine faculty honored as among Top Docs 2024 by Seattle Magazine
Nine UW Medicine Ophthalmology faculty members have been honored as being among Seattle’s Top Docs for 2024 by Seattle Magazine in its July 2024 issue. Seattle Magazine has published a list of the region’s top doctors for over two decades. None paid to be included, and all were nominated by their peers.
UW Ophthalmology faculty honored as Top Docs by Seattle Magazine are:
Michelle Cabrera, MD (pediatrics); Professor; Division Director, Pediatric Ophthalmology
Christopher Chambers, MD (oculoplastics); Associate Professor; Division Director, Oculoplastic and Reconstructive Surgery
Philip Chen, MD (glaucoma); Professor; Grace E. Hill Endowed Chair; Vice Chair for Clinical Services, Chief of Ophthalmology, Harborview Medical Center
Shu Feng, MD (comprehensive), Assistant Professor; Director of Medical Student Education
Courtney Francis, MD (neuro-ophthalmology); Associate Professor; Division Director, Neuro-Ophthalmology; Medical Director, UW Medicine Eye Institute
Eugene May, MD (neuro-ophthalmology); Clinical Associate Professor
Raghu Mudumbai, MD (glaucoma and neuro-ophthalmology); Associate Professor; Division Director, Glaucoma
Russell Van Gelder, MD, PhD (uveitis); Boyd K. Bucey Memorial Professor And Chair, UW Medicine Department of Ophthalmology; Director, Roger and Angie Karalis Johnson Retina Center; Director, UW Vision Science Center
Jennifer Yu, MD, PhD (comprehensive); Clinical Associate Professor; Director, 4W Ophthalmology Clinic at Harborview; Director of Trauma and Consult Services at Harborview
Education Spotlight:
Clerkships give medical students a quality introduction to ophthalmology
Each year, medical students from the UW and elsewhere spend two to four weeks doing an ophthalmology clerkship.
“It gives them an opportunity to learn about ophthalmology,” said Assistant Professor Shu Feng, MD, director of medical student education. “A clerkship is an elective for students in the UW School of Medicine that may be interested in ophthalmology or just expanding their knowledge of the eyes.”
During their clerkship, the students learn exam techniques, take a history, and do consults in the ER or in the hospital.
“They get to spend time with our faculty physicians and residents, getting a broad exposure to the work in the Eye Institute and the 4-West clinic at Harborview,” Dr. Feng said.
The clerkship gives them the complete picture of what an ophthalmologist does so that if they go into another specialty, they will know how to diagnose an eye problem or when to refer the patient to an ophthalmologist.
Clerkships are offered at several locations, including Harborview, Seattle Children’s, the Seattle VA Medical Center, and community sites in the WWAMI region.
For those medical students interested in an ophthalmology residency at UW, the clerkship is a “chance to recruit great students and see if it is a fit for them and us,” Dr. Feng said.
There are also clerkships available to medical students from outside the UW interested in applying for residency here. Dr. Feng herself was a visiting scholar at UW as a medical student at Oregon Health Sciences University before doing her residency here.
“I remember meeting (Professor Emeritus) Dr. (Robert) Kalina and many of the faculty and residents. It really gave me a sense of what it is like to come here for residency,” she said.
In addition to experience in the hospital and clinics, each medical student must present a case to Dr. Feng and others about a patient they saw and what they learned about their eye problem.
“The clerkship program is a great way for us to support our medical students and teach them about eye conditions so as doctors, they can appropriately know the basics of any common eye complaint or eye emergency,” Dr. Feng said.
To learn more about the UW Ophthalmology Clerkship Program, visit the department website here.

Welcome to our new Fellows!
Kinyoun Retina Fellow Dr. Alyssa Bonnell completed her residency here at UW in June. She was born and raised in Princeton, NJ.
She graduated from the University of Pennsylvania in Philadelphia, PA, with a Bachelor of Arts in Health and Societies: Public Health. After graduation, she moved to Seattle, where she enjoyed working with clay and glaze as a ceramic artist before attending medical school at Rutgers Robert Wood Johnson Medical School in New Brunswick, NJ.
As a medical student, Dr. Bonnell’s interest in ophthalmology and vitreoretinal surgery grew under the mentorship of Jonathan Prenner, MD, at NJRetina in New Brunswick, NJ. In her free time, Dr. Bonnell enjoys exploring Seattle’s coffee shops and restaurants, attending spin classes with friends, and spending time in the mountains with her husband and their two dogs.
Pediatric Ophthalmology Fellow Dr. Mennatullah Elfwwal was born and raised in Cairo, Egypt. She obtained her medical degree from Cairo University and completed her residency at Kasr Alainy Hospital in the Ophthalmology Department at Cairo University. In May 2020, she earned a master’s degree in Ophthalmology and completed short-term training programs at both the University of Missouri and Indiana University.
Dr. Elfwwal's multifaceted approach to ophthalmology and dedication to patient care, education, and research embodies her commitment to positively impacting the field and improving the lives of those she serves.
Outside of medicine, Dr. Elfwwal enjoys spending time with her family in the scenic parks of Seattle. She is also an avid enthusiast of the arts and enjoys swimming.
Gensheimer Fellow in Ocular Inflammatory Diseases/Uveitis Dr. Gunay Uludag Kirimli is originally from Turkiye.
She earned her medical degree at Istanbul University, Cerrahpasa Faculty of Medicine. It was during her residency at Istanbul University, Istanbul Faculty of Medicine, that her passion for uveitis and posterior segment diseases started.
Building on this interest, she pursued a research fellowship at Stanford University, Byers Eye Institute, focusing on clinical research in uveitis. She then completed a Medical Retina Fellowship at Duke Eye Center. She is excited to join the uveitis team at the University of Washington in Seattle for specialized training. Outside of work, Dr. Kirimli enjoys listening to music, traveling, and spending time with her husband and daughter.
Welcome to our new Residents!
Welcome to our first-year residents in the Class of 2028. Learn more about them on our Current Trainees page.
Dr. Micah Buckmiller was raised in Sandpoint, ID. He received his undergraduate education at Boise State University, where he studied chemistry with an emphasis on biochemistry. Upon graduation, he became interested in ophthalmology while working at Envision, Idaho’s eye bank, to recover corneal tissue for transplant. He attended medical school at the University of Washington School of Medicine through Idaho WWAMI and is excited to stay in the Pacific Northwest for an ophthalmology residency. Dr. Buckmiller enjoys rock climbing, mountain biking, disc golf, chess, crossword puzzles, coffee, and traveling in his free time.
Dr. Luke Harrison is a born and raised Washingtonian who grew up in both Whidbey Island and Tri-Cities. He stayed in the Pacific Northwest for his undergraduate education at Seattle Pacific University, participating in the debate team.
Prior to medical school, Luke worked as an ophthalmic technician and completed an advocacy internship with the American Academy of Ophthalmology. Luke was part of the Spokane cohort of the UW School of Medicine for medical school. In his free time, Luke enjoys traveling, cooking, and spending time with his wife and family. He is excited to stay in Seattle for residency and hopes to practice in a rural WWAMI area.
Dr. Karolina Leziak was born and raised in the Chicago area. She pursued her undergraduate studies in Neuroscience at Northwestern University. Before entering medical school, she researched disparities in care among low-income pregnant individuals. She then attended the University of Michigan Medical School, where she discovered her love for ophthalmology after witnessing its tangible impact on patients’ lives.
Dr. Leziak is thrilled to join the University of Washington for her ophthalmology residency. She is eager to merge her interests in neuroscience and healthcare disparities research to improve eye care accessibility for all patients. In her free time, you can find Dr. Leziak reading, spinning, hiking, playing tennis, and exploring her new hometown of Seattle!
Dr. Emma Stenz was raised in Dixon, CA, a small suburb of Northern California, alongside her younger sister. She attended Pepperdine University in Malibu, CA, after being accepted into the Regents’ Scholars Program, an academic scholarship program that further integrates students into liberal arts studies. She graduated summa cum laude in 2019 with a degree in Biology and a minor in Chemistry with the intent to apply to medical school following a gap year.
During her gap year, she worked for a retina clinic in Austin, TX, where she first discovered her love for ophthalmology and interest in entering the field. She attended McGovern Medical School at UTHealth Houston. She is thrilled to have the opportunity to return to the West Coast, this time up north in the PNW, for residency and to dig into her dual passions for the outdoors and ophthalmology.
Dr. Kevin Toolan was born in New York City but raised in a suburb of Chicago.
He graduated from the University of Michigan – Ann Arbor with a B.S. in Biology. He was first exposed to the wonders of ophthalmology as an undergraduate working in a bench research lab at the Kellogg Eye Center, where he completed an honors thesis. He returned to Chicago to attend medical school at Rush Medical College.
Dr. Toolan is the middle child of a family of five. He and his fiancée, Amy, are looking forward to exploring all the beauty that the PNW has to offer. He is especially excited to train at Harborview Medical Center, where his father, his greatest mentor, once cared for patients during his own orthopedic fellowship. Kevin enjoys intramural sports, skiing/snowboarding, and trying new restaurants/cuisines in his free time.
InSight Newsletter Spring 2024
Spring 2024
Message from the Chair

Welcome to the Spring 2024 edition of the Department of Ophthalmology InSight Newsletter. As our 2023-24 academic year nears its close, we look forward to the 50th annual Resident Alumni Day on Saturday, June 15, at the South Lake Union campus. Raj Apte, MD, PhD from Washington University will be our keynote speaker as the Roger Johnson Macular Degeneration Award winner this year. We are also starting a new feature for RAD this year, honoring a distinguished alumnus from our program for their contributions with an Alumni Spotlight lecture. Matt Oliva, MD (residency class of 2003) will be our inaugural speaker and provide insights into his many years of service with the Himalayan Cataract Project.
The research spotlight in this issue shines on Research Associate Professor Ethan Buhr, PhD. The Buhr Lab in the Vision Science Center at South Lake Union has identified additional unique photoreceptors, called opsins, that allow for the cells within the retina to synchronize with sunlight.
In our patient care feature, learn more about our oculoplastic and reconstructive surgery team and their remarkable work caring for many of our most complex cases.
In our education spotlight, our faculty and residents have been active in the greater Seattle community, providing compassionate care to the unhoused and underserved and inspiring young students to consider careers in ophthalmology.
Finally, in our philanthropy spotlight, learn more about the more than 50 years of partnership between the department and the University-Ballard Lions Club. Congratulations to their club on celebrating its centennial and we deeply appreciate the Lions’ commitment to preserving vision.
On behalf of the department, thank you for your continuing support of our mission to alleviate suffering from eye disease. Please visit our website at ophthalmology.washington.edu and our new Facebook and Instagram pages for more news and updates.
Russell N. Van Gelder, MD, PhD,
Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Director, Roger and Angie Karalis Johnson Retina Center
Director, Vision Science Center
Research:
Harnessing the healing power of light
A daily dose of light is essential and beneficial to our health, according to Research Associate Professor Ethan Buhr, PhD. Dr. Buhr recently gave an inside look at his research at the South Lake Union campus, followed by a tour of the Vision Science Center.
Buhr said light affects us in nonvisual ways, and the fact that wavelengths of light are present outdoors but lacking in indoor lighting might impact health.
"Our eyes and bodies can detect light far beyond what our visual system sees. Our brains, skin and eye surface can all anticipate sunrise and sunset independently, using light triggers, because of a non-visual connection with our eyes,” Buhr told the group. “This helps coordinate healing pathways so our skin and eye surface can repair wounds while minimizing UV damage, scarring, and infection.”
Dr. Buhr said our behavior and cellular biology synchronize with the 24-hour light cycles produced by the daily rising and setting of the sun. This is achieved through non-visual photoreception or the activation of photoreceptors that function independently of vision. Circadian clocks are present in nearly every cell. To synchronize sleep-wake cycles, our retinas transmit light information to our brain's central circadian clock using rods, cones and intrinsically photoreceptive ganglion cells.
The Buhr Lab in the Vision Science Center at South Lake Union has identified additional unique photoreceptors, called opsins, that allow for the cells within the retina to synchronize with sunlight. These photoreceptors are separate from visual photoreceptors, like an extra eye for the retina itself. The synchronization of circadian clocks within the retina contributes to the retina’s response to photodamage and the long-term health of the tissue.
In future studies, his laboratory will study how opsins’ input to the brain controls these seasonal changes and how this influences the rhythms of our internal organs.
Outside of the retina, the Buhr Lab is also studying the role of non-visual photoreceptors in other areas exposed directly to light, such as the cornea and skin. Violet-light-sensitive photoreceptor cells are induced in response to injury. Once active, these cells activate pathways related to the synchronization of wound-healing mechanisms. An important next step is understanding how the signal is transmitted among the cells.
Learn more about Dr. Buhr's research on the Department website.
An Illinois native, Dr. Buhr earned his Ph.D. in neuroscience at Northwestern University. He completed his postdoctoral training at the UW with Bucey Chair Dr. Russell Van Gelder. He joined the faculty in 2015. Dr. Buhr lives in Seattle with his wife and two children.
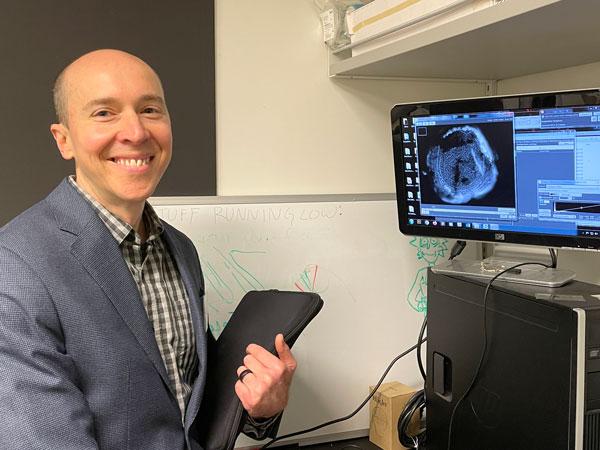
Patient Care:
Oculoplastic and Reconstructive Surgery
Of the major subspecialties in ophthalmology, oculoplastic and reconstructive surgery are among the most varied in their scope.
“There is significant variability in the procedures we do and the pathology we treat,” said Christopher Chambers, MD, Associate Professor and Division Director of Oculoplastic and Reconstructive Surgery in the UW Department of Ophthalmology. “This includes craniofacial surgery, cancer resection and reconstruction, trauma, cosmetic surgery, and functional defects of the eye, orbit, and tear ducts. Often, the pathology is more acute and can often be a systemic disease.”
The oculoplastic division includes Dr. Chambers, Assistant Professor Matthew Zhang, MD, and Clinical Associate Professors AJ Amadi, MD, and Holly Chang, MD, who practices at the Veterans Affairs Puget Sound Health Care System. Alexa Van Brummen, MD, is the current Hargiss Oculoplastic Fellow.
Dr. Chambers practices at the Eye Institute at Harborview Medical Center, the 4-West Ophthalmology clinic at Harborview, and Seattle Children’s Hospital, focusing primarily on cancer reconstruction, tumors, trauma, and pediatric eyelid and eye socket disorders. Cosmetic procedures such as face lifts, resurfacing, and eyelid lifts are a small part of the practice.
“I enjoy the variety of the surgeries we do and the pathology we see, caring for acutely sick people and giving them excellent care that they wouldn’t get elsewhere,” Dr. Chambers says.
The work is often interdisciplinary, with other craniofacial trauma surgeons collaborating with the oculoplastic team to treat the same patient.
Ophthalmology is something of a family business for Dr. Chambers — his wife Yasmin is an oculoplastic surgeon, his father is a retina specialist, and his sister is a glaucoma specialist. Raised in Columbus, Ohio, he received his medical degree from Ohio State University, completed residency in ophthalmology at the Kresge Eye Institute, and fellowship in oculoplastic and reconstructive surgery at the University of Pennsylvania. Dr. Chambers and his wife are the parents of three young daughters.
Before joining the UW faculty in 2015, Dr. Chambers was a faculty member at Northwestern University, Feinberg School of Medicine. He was the associate residency program director and won the medical school teaching award while on staff. Dr. Chambers served as a team physician for the NHL Chicago Blackhawks and also treated players from the MLB Chicago Cubs.
Dr. Chambers is also the director of the oculoplastic and reconstructive surgery fellowship and associate residency director for the department.

Education:
Faculty, residents team up for community outreach
Department of Ophthalmology faculty and residents recently participated in two inspiring community outreach activities.
The first was “Doctor for a Day,” an outreach program for youth of color in the greater Seattle area. The aim is to encourage middle and high school students to consider medicine or other healthcare careers.
Organized by UW School of Medicine students, Doctor for a Day events comprise hands-on stations. Ophthalmology faculty and residents offered three tables for the students to explore vision testing, color vision, stereopsis, suturing practice, viewing the retina with indirect ophthalmoscopes, viewing their retina with a camera, and other fun items like a cataract and AMD simulator.
Doctor for a Day focuses on increasing the number of underrepresented students in health professions. Research shows that without intervention in elementary school, underrepresented students may lose interest in science and math by their teens and discount their abilities in those subjects before finishing high school.
More than 100 students in grades K-12 participated in the event in the Health Sciences Education Building on the Seattle campus. The neurosciences and pathology departments also participated.
Representing the Ophthalmology faculty were Drs. Karine Duarte Bojikian, Shu Feng, Laura Huang, Miel Sundararajan, and Jennifer Yu were joined by residents Drs. Johnson Huang, Nicole Mattson, and Ryan Yanagihara.
For more information about the Doctor for a Day program, visit their web page.
Assistant Professor Miel Sundararajan, MD, and residents also participated in the Seattle/King County Clinic, which brings together healthcare organizations, civic agencies, non-profits, private businesses, and volunteers from across the State of Washington to produce a giant free health clinic at Seattle Center. The four-day volunteer-driven clinic provides free dental, vision, and medical care to anyone in the region who struggles to access or afford healthcare.
The clinic provided more than $2.6 million in comprehensive healthcare to over 2,900 people. In its nine years of operation, the Clinic has provided free healthcare to more than 30,000 patients who have fallen through the region’s healthcare gaps. All were unable to afford or access the care they were seeking elsewhere.
For more information about the Seattle King County Clinic program, visit their web page.

Philanthropy:
University-Ballard Lions Club celebrates 100 years of service to the community
The University-Ballard Lions Club will celebrate its centennial with a gala luncheon on June 6. The UW Department of Ophthalmology will be a presenting sponsor for the event.
The Lions’ support for vision research is legendary; since 1925 when Helen Keller asked the members of Lions Clubs International to become her “Knights of the Blind.” Since then, hundreds of millions of lives have been changed through the vision-related work of Lions around the world, and today, the worldwide association is as dedicated as ever to hastening the day when no one should suffer unnecessarily from vision problems. Through eye centers and hospitals, medicines and surgeries, eyeglasses, and eye banks, Lions are working to end preventable blindness and aid the visually impaired.
The University Lions Club, which has merged with the Ballard Lions Club, began its support for the UW Department of Ophthalmology by creating the Lions Eye Bank more than 50 years ago. Rebranded in the 2000’s as SightLife, this eyebank has grown into one of the world’s largest, providing corneal tissue for surgeons throughout the US and throughout the world.
“The Lions supported the Eye Bank, which provided corneal tissue for many transplants,” said Donna Oiland, who became its director in 1972. “So many people had their vision restored, and it is amazing how this all came about with the partnership between Lions and the UW.”
Dr. Fred Minifie recalled how the relationship between Lions and the Department grew over the 27 years Dr. Robert Kalina was chair and has continued to grow during Dr. Russell Van Gelder‘s 17 years as chair of the Department of Ophthalmology.
“Bob Kalina had such a large influence in the early development of the Lions Eye Bank as its medical director. Ultimately, the Eye Bank grew and became too large to remain in the Department. When Russ Van Gelder arrived in Seattle, he was instrumental in developing several linkages to Seattle-area Lions Clubs,” said Minifie, who would later chair the UW Medicine Eye Institute Community Action Board.
When Siddall Chair Tueng Shen, MD, PhD, came to UW in the early 2000s, the University Lions Foundation supported her research with a grant. She held the title of the Northwest Lions Professor of Ophthalmology for several years until she received her current endowed chair position. Minifie recalled Dr. Shen's research on developing artificial corneas, including going to her native China and implanting them in patients there. The University-Ballard Lions Club “has been truly proud to support Dr. Shen’s work over these many years,” he said.
In recent years, the Lions have presented an annual Helen Keller Award to a researcher at the annual Gained in Translation conference. Gained in Translation is a meeting of clinicians and vision scientists from the University of Washington, the University of British Columbia, and Oregon Health Sciences University. Presentations focus on bridging the gap between disease treatment and the latest translational and basic research advances.
The Lions Gift of Sight program through the Department provides used eyeglasses to patients who may not be able to afford them and helps with the cost of scleral lenses for cornea patients. To donate to this fund, visit give.uwmedicine.org.
InSight Newsletter Winter 2024
Winter 2024
Message from the Chair
Welcome to the Winter 2024 edition of the Department of Ophthalmology InSight Newsletter. Our research, educational, and clinical activities are bustling right now, and in this newsletter, we are pleased to highlight several areas.

The research spotlight in this issue shines on Assistant Professor Debarshi Mustafi, MD, PhD, and his lab’s exciting and groundbreaking work to create a method for rapid genetic sequencing for inherited retinal diseases, reducing the time by weeks in some cases.
In our patient care feature, we celebrate the fifth anniversary of the Karalis Johnson Retina Center at South Lake Union.
This center, supported by a remarkably generous gift from Angie Karalis Johnson, opened in 2019. It has supported over 32,000 patient visits in the past five years and an ambitious research program. Angie’s dream for the Karalis Johnson Retina Center to become the world’s leading center for the cure and treatment of retinal diseases is coming ever closer to reality. Read more about the center and its work in our special 5-year Community Report.
In our education spotlight, meet our incoming fellows for 2024-25 joining us in July and learn more about the research of first-year resident Deborah Im, MD, who received special recognition at the annual meeting of the American Academy of Ophthalmology.
Finally, in our philanthropy spotlight, learn more about Larry and Eileen Tietze, who have made annual gifts from their family foundation in the form of an award to support the work of an early-career or mid-career scientist in the UW Department of Ophthalmology.
On behalf of the department, thank you for your continuing support of our mission to alleviate suffering from eye disease. Please visit our website at ophthalmology.washington.edu and our new Facebook and Instagram pages for more news and updates.
Russell N. Van Gelder, MD, PhD,
Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Director, Roger and Angie Karalis Johnson Retina Center
Director, Vision Science Center
Research
Rapid genetic sequencing for inherited retinal disease with new testing panels
When attempting to identify the sequence of the genes responsible for inherited retinal diseases (IRDs), time is of the essence. Whereas previously, this process could take months, Assistant Professor Debarshi Mustafi, MD, PhD, and his colleagues in the UW Department of Ophthalmology have developed a method for genetic sequencing for IRDs that takes just days.
Mustafi, a pediatric retina specialist at Seattle Children’s with a lab at the Karalis Johnson Retina Center at South Lake Union, is investigating the genetic basis of inherited retinal degeneration and the potential for therapeutic intervention to prevent the progression of blindness. In the pediatric population, IRDs constitute a significant cause of visual impairment and can be one of the first presenting features of a syndromic condition with extra-ocular consequences.
Using isolated blood samples from affected IRD patients and their families, the lab performs targeted genome sequencing to identify novel pathogenic variants of disease and reconstruct disease haplotypes, with implications for interpreting disease risks in IRDs.
The molecular basis of IRDs requires effectively characterizing mutations across over 300 genes. Mustafi said that currently used short-read panel sequencing leaves 30–40 percent of patients with a non-diagnostic result. This is because smaller commercial panels do not cover all regions of disease genes. Targeted long-read sequencing can focus the sequencing efforts of disease regions of interest to provide comprehensive information on genetic variants contributing to disease.
Mustafi and his colleagues are now targeting “every gene implicated in causing disease” related to IRDs, enabling sequencing as many as 373 genes in one sequencing run.
“This sequencing has the potential to enable rapid, phased mutation analysis in a single step in a matter of days or hours,” he said. “The sequencing is customizable. It takes a matter of minutes to add or subtract a gene. This way, we can selectively sequence what we want and disregard everything else.”
The rapid turnaround from sample extraction to diagnosis will enhance clinicians' ability to provide more targeted therapy in a timely manner.
Mustafi is also investigating the potential of this technique to rapidly identify pathogenic variants in retinoblastoma, for which rapid diagnosis is critical as it can affect treatment regimens to minimize morbidity and mortality.
“Not only are we able to provide a complete molecular diagnosis in a shorter time frame, but we can do so at nearly a quarter of the cost of commercial panels and using only the blood from the patient,” Mustafi said. “The goal is to determine if we can identify variants quickly and think about the next step, knowing their disease variant we can target.”
Rapid sequencing is currently used to diagnose eye diseases such as Usher Syndrome, Stargardt disease, and retinitis pigmentosa. But there is potential to expand this to other ocular diseases and even extra-ocular inherited conditions, Mustafi said.
“We want to make the targeting sequencing more efficient and increase our ability to find rare variants,” he said. “This should also work on any Mendelian disease outside of ophthalmology.”
Dr. Mustafi grew up in Chicago and earned his bachelor’s degree with Honors in Chemistry from the University of Chicago. He then enrolled at Case Western Reserve University as part of the NIH Medical Scientist Training Program to earn his MD and PhD.
Upon completing his internship, he completed his ophthalmology residency at the University of Southern California/LA County. Upon finishing residency, he was awarded the prestigious Heed Fellowship and completed his medical and surgical vitreoretinal fellowship at the UW before joining the faculty.

Patient Care
Karalis Johnson Retina Center celebrates five years
January marked the fifth anniversary of the Roger and Angie Karalis Johnson Retina Center opening at South Lake Union.
This center, supported by a remarkably generous gift from Angie Karalis Johnson, opened in 2019. It has supported over 32,000 patient visits in the past five years and an ambitious research program.
Angie’s dream for the Karalis Johnson Retina Center to become the world’s leading center for the cure and treatment of retinal diseases is coming ever closer to reality.
Her dedication to helping those with eye disease is phenomenal, said Russell Van Gelder, MD, PhD, Professor and Bucey Chair of the Department of Ophthalmology. “This is her vision. This is the work of Angie and Roger, and it extends the legacy of Roger and her late parents.”
Learn more in this special 5-year Community Report about how the Karalis Johnson Retina Center (KJRC) supports four pillars of research in its mission to eradicate retinal blindness: advanced optics imaging, computational ophthalmology, accelerating the therapeutic pipeline, and vision restoration research.
“I always had this in my mind that someday I can help some of these people to keep from going blind,” she said. “I knew from working alongside Roger the potential of what this means - not just another center, but to create a beacon of light for those patients.”
UW vision scientists are committed to improving diagnosis and treatment and ultimately finding cures for retina diseases. The department ranks third in the nation in NIH funding among ophthalmology departments, and the UW is second for National Eye Institute funding. Most of this research is based at the Karalis Johnson Retina Center.
“So many people who suffer from retinal disease benefit from this center. We are at a point where the science can move treatment of these diseases,” said Dr. Van Gelder. “At the KJRC, we have brought everything together in one place to optimize patient care and treatment.”
The KJRC is a major referral center, seeing patients from the five-state WWAMI (Washington, Wyoming, Alaska, Montana, Idaho) region.
“We continue to provide many services not found in the community, including managing eye cancer (ocular oncology), uveitis, and medical and hereditary retinal disease,” Dr. Van Gelder said.

Education
First-year resident receives honor for research paper at AAO meeting
First-year Ophthalmology resident Deborah Im, MD, was recently honored for a research paper she was first author and co-wrote while in medical school at the Keck School of Medicine, University of Southern California. She presented the paper at the annual meeting of the American Academy of Ophthalmology (AAO) in San Francisco, and it was selected as the best podium presentation at that AAO session.

“It was a surprise,” Im said. “I had forgotten that they gave such an award. I was the only junior resident that presented during that session.”
The paper, “A Multicenter Analysis of Nucleic Acid Quantification Using Aqueous Humor Liquid Biopsy in Retinoblastoma,” was published in Ophthalmology Science in February 2023. One of the co-authors was Andrew Stacey, MD, associate professor of ophthalmology and an ocular oncology specialist.
Retinoblastoma is the most common ocular cancer in children. It can only be diagnosed by viewing the eye and not via biopsy because of the risk of metastasis. This study investigated using aqueous humor (AH), the fluid in front of the eye, as a surrogate tumor biopsy.
“Four different children’s hospitals sent us aqueous humor samples from children with retinoblastoma, and from children without retinoblastoma,” Im said. It was the first large and multicenter study, with 125 samples, investigating aqueous humor liquid biopsy in retinoblastoma.”
The study concluded that aqueous humor was a reliable source of genetic material in children with retinoblastoma. Further, genomic analysis of aqueous humor may be helpful in diagnosing active retinoblastoma disease, especially when the view to the eye is obstructed, such as when there is blood or cataract in the eye.
Im attended the Keck School of Medicine at USC. She completed a research year with the Wright Foundation and her mentor Jesse Berry, MD, after her third year of medical school.
“I was interested in ophthalmology because vision is a complicated pathway and there is a lot of gratification working with patients to protect and care for their sight,” Im said. “I did a rotation as a medical student and enjoyed the precision of it and being able to visualize the pathology and the possibility to intervene with surgery.”
Raised in the Pasadena area, she studied microbiology at the University of California, Santa Barbara.
“I didn’t initially think I would go to medical school, but I knew I wanted to work with people and have a great impact through my education. I am so happy to be at the University of Washington. I rotated here as a medical student, and my experience here has been amazing because of my co-residents and our faculty being so invested in our teaching.”
Fellows announced for 2024-25
We are pleased to announce that these incoming fellows will join us in July 2023.
Pediatric Ophthalmology: Mennatullah Elfwwal, MD, Cairo University in Egypt.
Kinyoun Retina Fellowship: Alyssa Bonnell, MD, is currently completing her residency here at UW.
Gensheimer Endowed Fellowship in Ocular Inflammatory Diseases/Uveitis: Gunay Uludag Kirimli, MD, is completing a medical retinal fellowship at the Duke Eye Center after serving as a research fellow at Stanford and residency at Istanbul University in Türkiye.
We are also excited to share fellowship match results for our UW fourth-year residents graduating this summer.
Hannah Hashimi, MD, will pursue a pediatric fellowship at Duke University.
Alekya Rajanala, MD, will pursue a cornea fellowship at UC San Francisco.



Class of 2028 residents will join the Department of Ophthalmology in July

Philanthropy:
Eileen and Larry Tietze: Backing promising scientists, one award at a time
Investing in people and great ideas has been a hallmark of Eileen and Larry Tietze’s philanthropy for over 20 years.
Their philosophy was shaped by Larry’s father, John Herman Tietze. John was an ardent advocate for education and helped to sponsor scholarship funds at Kansas State University. In his later years, John supported biomedical researchers at the Mayo Clinic. Eileen recalls John’s reflections on philanthropy: “My one wish is to back the young men and women at the bench. They have big ideas, energy, and enthusiasm.”
That is precisely what Larry and Eileen have done through the Tietze Family Award for Vision Sciences since 2010. After an introduction to Bucey Memorial Chair Russell Van Gelder, MD, PhD, the Tietzes have made annual gifts from their family foundation in the form of an award to support the work of an early-career or mid-career scientist in the UW Department of Ophthalmology.
Bergy Professor Jennifer Chao, MD, PhD, vice-chair of research, says, “Many new investigators require bridge funding until they obtain major grants. Sources of philanthropic funding like the Tietze Family Awards are critical in filling in the gaps for scientists beginning their careers.”
“A grant of $30,000 or $40,000 may seem modest,” Eileen Tietze notes, “But it is significant if you are a researcher at a crucial point in your career and need funding.”
The Tietze Family Awards have supported several vision science researchers, including:
- Jennifer Chao, MD, PhD, studying stem cell approaches to studying macular degeneration disease process;
- Jay Neitz, PhD, and Maureen Neitz, PhD, exploring gene therapy methods to treat macular degeneration and color blindness;
- Andrew Stacey, MD, MS, leveraging machine learning to detect rare eye cancers with imaging at earlier stages of disease and
- Ethan Buhr, PhD, understanding photoreceptors in the visual system.
“We are willing to fund riskier projects or ideas. At the very least, the scientists will learn something after trying a new method or approach. We have been impressed by the quality of the research scientists and their important discoveries that could improve care for patients suffering from blinding eye diseases,” Larry and Eileen Tietze say.
“If we had one wish that could be granted, it would be that more people would recognize this model of philanthropy can be effective. Leveraging seed money gives gifted scientists a real chance to make progress at the bench and compete for major grants. And it has been rewarding to see our grants yield more investments.”
The Tietze Family Awards' initial investments have helped vision science researchers earn subsequent government, foundation, and private donor funding.
In addition to their support in the UW Department of Ophthalmology, Larry and Eileen Tietze have also directed generous gifts to support research in the Institute for Stem Cell and Regenerative Medicine and the Department of Allergy and Infectious Disease.

InSight Newsletter Fall 2023
Fall 2023
Message from the Chair

Welcome to the Fall 2023 edition of the Department of Ophthalmology InSight Newsletter. In the rhythms of our department life, during the fall, we fully engage in all aspects of our mission, including our research, educational, and clinical activities.
The research spotlight in this issue shines on Associate Professor Mike Manookin, PhD, and his lab’s work to understand the computational circuitry of the retina. His work will be critical to efforts to restore vision in the coming years.
In our patient care feature, we introduce three new faculty who joined us this fall – Assistant Professors Brian Chou, MD, MA; Tony Chung, MD; and Chris Fortenbach, MD, PhD.
In our philanthropy feature, learn about how Suzanne Ragen has supported our department through her volunteer work with the Community Action Board and, most recently, her generous support for the establishment of the Brooks and Suzanne Ragen Endowed Faculty Fellowship in Ophthalmology this year.
Our department is proud of our fellowship programs. In our education feature, meet Dr. Jeannette Stallworth, this year’s pediatric ophthalmology fellow, a Bellevue native who has come home for her subspecialty training.
On behalf of the department, we wish you and your families the very best this holiday season. Please visit our website at ophthalmology.washington.edu and our Facebook page for more news and updates.
Russell N. Van Gelder, MD, PhD,
Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Director, Roger and Angie Karalis Johnson Retina Center
Research: Manookin Lab is furthering understanding of the retina
Finding a way to restore vision lost to eye disease is the overarching goal of Associate Professor Mike Manookin’s research at the Vision Science Center at South Lake Union.
“The goal is to understand the retina well enough to restore vision in disease states,” says Manookin. “We currently don’t have a deep enough understanding of the retina to restore function following blinding disease.”
To do that, we need to know the retina's circuitry, Manookin explained.
“There's been progress made in some animal models, but less so in humans in learning what information different retinal circuits are encoding and how disease affects them,” he says.
The Manookin laboratory investigates the function and connectivity of neural circuits in the retina using techniques including electrophysiology, calcium imaging, and electron microscopy.
Working in collaboration with Research Associate Professor Ethan Buhr, PhD, and Adjunct Professor Fred Rieke, PhD, Manookin is recording the electrical activity of light sensitivity in neurons of the retina to help learn how we can stimulate light sensitivity. His research is partly supported by grants from the National Institutes of Health.
Manookin says there are over 80 different neuronal types in the human retina. These form the components of the specialized circuits that transform the signals from photoreceptors into a neural code responsible for our perception of color, form, motion, and, thus, visual experience.
Many blinding diseases, such as retinitis pigmentosa, cause death of the rods and cones but spare other cell types within the retina. Thus, many techniques for restoring visual function following blindness are based on the premise that other cells within the retina remain viable and capable of performing their various roles in visual processing. However, the circuitry of the remaining retina does seem to change following the loss of photoreceptors. Understanding the native and non-native circuitry will be critical to emerging techniques for vision restoration, including gene therapy, cell-based therapies, and small molecule photoswitches.
Raised in a farming area of central Utah, Mike completed a mission for his church in Estonia. He studied linguistics as an undergraduate at Brigham Young University before becoming interested in neuroscience. At the University of Michigan, studying for his PhD, he “really got hooked on vision,” studying visual coding in the retina and physiology of the retina.
He came to UW as a post-doctoral scholar before joining the faculty of the Department of Ophthalmology in 2015. Mike and his wife Karen, a former faculty member in the School of Dentistry, have four children. In his free time, he enjoys cooking and reading.
Patient Care: Welcome to our new faculty members
The department welcomed three new faculty members on Sept. 1.
Assistant Professor Brian Chou, MD, MA, returns to our department after completing his ophthalmology residency at UW in 2022. He recently completed a neuro-ophthalmology fellowship at the Stein/Doheny Eye Institute at UCLA. He grew up in South Carolina before venturing to Chicago for his undergraduate and medical education at Northwestern University. He concurrently completed a master’s degree in Bioethics and Medical Humanities during his time at Northwestern. He enjoys staying active through rock climbing and partner dancing.
Assistant Professor Anthony Chung, MD, practices comprehensive ophthalmology and specializes in cataract surgery. He was born and raised in Ames, Iowa. He attended the University of Iowa, where he obtained his B.S. with honors in psychology and a minor in biology. He then received his medical degree from the Carver College of Medicine at the University of Iowa. He completed his internal medicine internship and ophthalmology residency at the University of Iowa Hospitals and Clinics. Dr. Chung served on the faculty of Case Western Medical School for several years before joining UW. Dr. Chung is an avid cook and enjoys traveling, hiking, and entertaining his two daughters with his wife, a member of the OB/GYN department faculty.
Assistant Professor Christopher Fortenbach, MD, PhD, grew up in Northern California, where he attended the University of California, Davis, for his undergraduate education. He stayed there to complete an MD/PhD program, where he earned his PhD in Biochemistry, Molecular, Cellular, and Developmental Biology, studying retinal physiology.
Dr. Fortenbach completed his ophthalmology residency and vitreoretinal surgery fellowship at the University of Iowa Hospitals and Clinics. He is an active clinician scientist with a laboratory studying how the retina encodes light and therapies to restore vision loss. In his spare time, Dr. Fortenbach enjoys spending time with his family, backpacking, cycling, tennis, and cooking.
Philanthropy: From art to the eyes - improving vision care and fueling research
Imagine you visit the Seattle Art Museum. Your experience will be visual, appreciating the art's color, texture, scale, and shape, as well as reading titles, captions, and background information.
Now imagine you visit the museum with a blindfold on. This is how our patients with low vision must experience art, and this is the challenge Suzanne Ragen faced as a docent in 2008 when visitors from Lighthouse for the Blind arrived at the museum. Having served as a volunteer docent since 1965, Suzanne is passionate about making art come alive for visitors. Yet she had never given a tour for individuals with low vision. When she better understood their needs for potential accommodations such as sight dogs, canes, magnifiers, and vivid audio descriptions of the room and the art, Suzanne founded Art Beyond Sight. She trained 15 docents to provide monthly tours at the Seattle Art Museum for individuals with low vision. For example, it needed to be more adequate to verbally describe the sculpture of Roman emperor Marcus Aurelius, noting details about his hair, toes, or bust. Low-vision visitors want to know details about lighting and the room where the sculpture was situated.
Suzanne’s appreciation for vision care and research has grown over the years. While her husband Brooks, who passed away in 2018, served on the UW Medicine Scholarship Development Committee, Suzanne began volunteering with the UW Eye Institute’s Community Action Board (CAB) in 2011. Suzanne learned about faculty-led research to prevent blindness and develop novel treatments for eye diseases. Along with others, Suzanne helped Bucey Chair Dr. Russell Van Gelder and fellow CAB volunteer Camille Jassny spread the word about UW Medicine’s excellent clinicians, researchers, and patient care through outreach talks throughout the Puget Sound region.
Motivated to help Dr. Van Gelder recruit and retain excellent clinicians and researchers committed to preventing blindness, Suzanne and her family established the Brooks and Suzanne Ragen Endowed Faculty Fellowship in Ophthalmology this year. She hopes this fellowship will significantly help the Department of Ophthalmology attract clinicians and scientists who drive innovative research and discoveries benefitting current and future patients. The first holder of the fellowship will be appointed and recognized in 2024.
We are grateful to Suzanne Ragen and the Brooks and Suzanne Ragen Family Foundation for their generous support. In addition to supporting research and faculty in ophthalmology, the Ragen family has supported scholarships for medical students at the UW School of Medicine for many years. Finally, named after Brooks and Suzanne Ragen, the annual Ragen Volunteer Service Award acknowledges the outstanding service from a volunteer, faculty, or staff member who advances the mission of UW Medicine to improve public health.
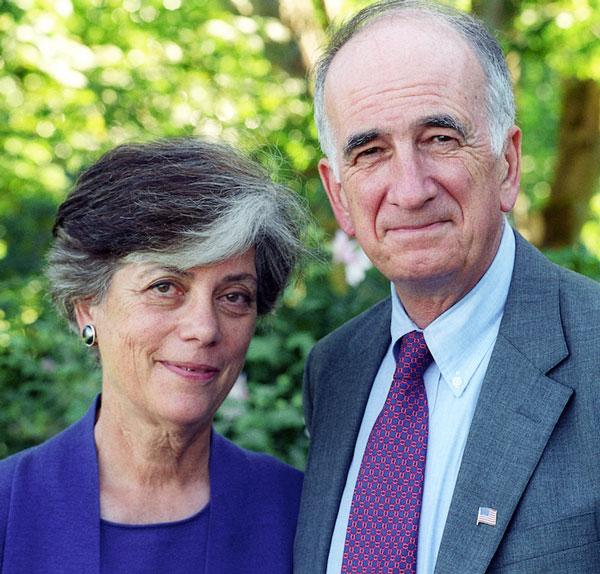
Education: Pediatric Fellowship is a homecoming for Dr. Jeannette Stallworth
As a Bellevue native, Dr. Jeannette Stallworth, the current Pediatric Ophthalmology and Strabismus fellow, is thrilled to serve in the area where she was raised.
Ophthalmology currently has four fellowships – Retina, Pediatric, Oculoplastics, and Uveitis. The Pediatric Ophthalmology and Strabismus Fellowship began in 2012, said Fellowship Director Associate Professor Erin Herlihy, MD.
“We are so pleased to have Jeannette here as our fellow this year,” she said. “There is a shortage of pediatric ophthalmologists nationwide, and we are glad she could come home to complete her training.”
Dr. Herlihy said the fellow participates in a wide range of clinical care and surgical procedures that comprise pediatric ophthalmology and adult strabismus, including pediatric cataract and glaucoma surgery, nasolacrimal and pediatric oculoplastic procedures, surveillance and treatment of retinoblastoma, retinopathy of prematurity (ROP), uveitis, and inherited retinal diseases. The fellow works collaboratively with many other pediatric subspeciality services at Seattle Children’s. The fellow also has the opportunity to interact with vision scientists at UW and Seattle Children's.
“One of the amazing parts of this pediatric fellowship program is the variety of experiences,” Stallworth says.
Her weeks are full, with numerous clinics and two days per week operating at Seattle Children’s, participating in retinopathy of prematurity rounds at both UWMC-Montlake and Seattle Children’s weekly, performing research, and additionally operating with Associate Professor Courtney Francis, MD, on adult strabismus cases twice a month. She also works with ocular oncology specialist Andrew Stacey, MD, and oculoplastics specialist Chris Chambers, MD, on their pediatric patients at Seattle Children’s. She has her fellow clinic and helps run the inpatient consult service.
Dr. Stallworth is participating in a research project with Dr. Michelle Cabrera, Associate Professor and Division Director, Pediatric Ophthalmology. Premature infants are at risk for ROP, a disease of the developing retina. Seattle Children’s pediatric ophthalmologists use advanced technology to noninvasively image newborn eyes with a handheld version of a technology found in most ophthalmology offices, Optical Coherence Tomography (OCT).
Dr. Stallworth graduated from Newport High School before attending Princeton University, graduating magna cum laude with a Bachelor of Arts in Economics. She then earned her medical degree from the Duke University School of Medicine.
“I had originally thought I might become a pediatrician, but it was as a medical student that I first became interested in ophthalmology,” she said. “I enjoyed surgery, and ophthalmology offers such a wide variety of cases.”
Dr. Stallworth completed her general surgery internship and an ophthalmology residency at the University of California, San Francisco, where she was awarded a Heed Fellowship.
Outside of work, Dr. Stallworth enjoys playing the cello, traveling, and spending time with her husband and eight-month-old daughter.
Visit the department website here to learn more about the department’s fellowship programs.

InSight Newsletter Summer 2023
InSight Newsletter | Summer 2023
Message from the Chair
Welcome to the Summer 2023 edition of the Department of Ophthalmology Insight Newsletter.

The research spotlight in this issue shines on Ricky Wang, PhD, George and Martina Kren Endowed Chair in Ophthalmology Research and Professor of Ophthalmology and Bioengineering, who has been selected as the 2023 UW Medicine Inventor of the Year, the school’s highest honor for innovation. The Inventor of the Year Award recognizes a UW researcher whose work has the potential to radically improve healthcare through the translation of research from the bench, with industry partnerships, to products or processes with significant impacts on health.
Ricky’s work in ophthalmology and bioengineering has been transformational, including the development of optical coherence tomography (OCT) angiography, a technique in which blood flow can be measured in all blood vessels in the eye non-invasively. This technique is now a standard testing modality in ophthalmology offices worldwide. He has also collaborated with Professor of Ophthalmology and Graham and Brenda Siddall Endowed Chair Tueng Shen, MD, PhD, on developing an OCT-based method to measure the cornea's structural integrity. Ricky is a beloved colleague in our department, and we are so proud to see him receive this honor.
In our patient care feature, you will learn about the work of one of our newest faculty members, Assistant Professor Miel Sundararajan, MD, a specialist in both cornea and uveitis who also leads our community outreach efforts. Last month Miel and Eye Institute staff performed vision testing of athletes at the Special Olympics in Tacoma. Our residents and fellows have joined her at other community health clinics throughout the Seattle area.
The Bishop Foundation has been a critical supporter of the department for many years, including the support of Bishop Professor Jay Neitz, PhD. Learn more about the Bishop Foundation in this spotlight on philanthropy.
Finally, in our education spotlight, our 49th annual Resident Alumni Day was held on June 17 with keynote speaker Kuldev Singh, MD, PhD of Stanford University, followed later that evening by our graduation honoring an outstanding group of departing fellows and residents.
Please visit our newly redesigned website at ophthalmology.washington.edu for more news and updates.
We hope you enjoy our summer update!
Russell N. Van Gelder, MD, PhD, Professor and Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Research: Ricky Wang, PhD to receive UW Medicine Inventor of the Year Award
Ricky Wang, PhD, George and Martina Kren Endowed Chair in Ophthalmology Research and Professor of Bioengineering and Ophthalmology, has been selected as the 2023 UW Medicine Inventor of the Year.
The UW Medicine Inventor of the Year award honors outstanding UW scientists whose inventions have significantly affected human health and our local economy. The Inventor of the Year Award recognizes a UW researcher whose work has the potential to radically improve healthcare through the translation of research from the bench, with industry partnerships, to products or processes with significant impacts on health. Selection is based on the researcher’s contributions to the bioscience sector and the UW faculty community and for contributions to the UW Co-Motion mission: to extend the impact of UW research through new partnerships that encourage investment in innovation.
“I am deeply humbled by this honor,” Dr. Wang said. “It has truly been my honor to work here at UW with so many brilliant colleagues in Bioengineering, Ophthalmology, and our lab.”
Dr. Wang is widely credited with inventing optical coherence tomography (OCT) angiography, a technique in which blood flow can be measured in all blood vessels in the eye non-invasively. This technique is now a standard testing modality in ophthalmology offices worldwide. His efforts have contributed to retinal findings in patients, including infants, with unprecedented precision, speed, and imaging resolution. He has also collaborated with Professor of Ophthalmology and Graham and Brenda Siddall Endowed Chair Tueng Shen, MD, PhD, on developing an OCT-based method to measure the cornea's structural integrity.
The School of Medicine and the University of Washington will honor Dr. Wang as the Inventor of the Year at a reception this coming fall, where he will receive an inscribed statuette and a $5,000 award.
The Wang lab is dedicated to developing novel and clinically useful biomedical imaging techniques for early diagnosis, treatment, and management of human diseases. By exploring the properties of light, tissue, and their interactions, the Wang lab invented, discovered, or pioneered a wide range of techniques, including optical microangiography, full-range complex Fourier domain optical coherence tomography, optical clearing of biological tissue, optical elastography, phase-sensitive optical coherence vibrometry, and multifunctional nanoparticle contrast agents. These methods have found broad application in fields ranging from imaging tissue morphology, tissue blood microcirculation (brain, retina, cochlea, skin, muscle, etc.), imaging tissue mechanical properties, and characterizing embryonic heart development.
At the outset of the pandemic, the Wang lab developed a smartphone-based technique to capture information such as oxygen level, pulse rate, respiratory rate, and blood perfusion and adapted their low-cost, camera-based optical sensing system to collect vital sign measurements from COVID-19 patients. Symptomatic and asymptomatic patients and health providers could use the system to assess the severity of the illness and help decide if they need hospitalization, reducing unnecessary burdens on hospitals.
Dr. Wang has been a UW faculty member since 2010. He is a joint Professor in both Departments of Ophthalmology and Bioengineering. In addition to the Kren Chair, Dr. Wang has also held the Washington Research Foundation and David and Nancy Auth Innovator Award in the Department of Bioengineering.
Dr. Wang earned his PhD in engineering from the University of Glasgow. He began his academic career in the United Kingdom, holding a professorship at Cranfield University. In 2005 he moved to Oregon Health Sciences University, where he directed the biophotonics and imaging laboratory.
Dr. Wang’s laboratory is phenomenally productive. He has authored or co-authored over 500 papers in peer-reviewed literature. He is currently editor-in-chief of Biomedical Optics Express journal.
Learn more about Dr. Wang's research at his lab website, https://depts.washington.edu/wangast/.
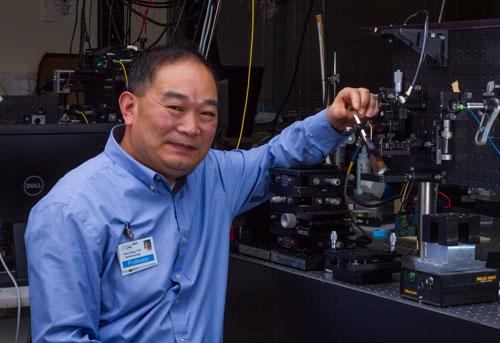
Patient Care: Miel Sundararajan, MD leads community outreach for Ophthalmology
Giving back to the community is an integral part of Dr. Miel Sundararajan’s mission as an ophthalmologist.
“I have always been involved in caring for the underserved and wanted to bring that here,” said Sundarajan, Assistant Professor and specialist in cornea and uveitis. “It’s exciting for me to be involved in broadening our outreach as a department.”
Dr. Sundararajan is the director of community outreach for the department. Under her leadership, trainees and staff have participated in several outreach activities over the past year.
These have included the twice-yearly Seattle-King County community clinic at Seattle Center. This four-day event includes medical and dental screenings at no cost to participants. Dr. Sundararajan was joined by residents and fellows who have gained valuable experience treating underserved populations.
In June, she was joined by Eye Institute staff to provide vision screening for participants in the Special Olympics at Pacific Lutheran University.
“The more that we do, the more people become aware of our ability to participate,” she said.
Born in Cuba, where her parents had lived for five years, Miel, which means honey in Spanish, moved to the US when she was two and was raised in South Bend, Ind. Her mother formerly taught at the Indiana University medical school and is now an emergency medicine physician.
“I always knew I wanted to be a doctor and do surgery,” she said. She completed an eight-year undergraduate and medical school program with Rice and Baylor, followed by residency in New York and fellowships in cornea and uveitis at the University of California San Francisco.
She decided on ophthalmology because of the diagnostics involved and the surgical element combined.
“What's exciting about cornea is that there is so much to be done to restore vision; my particular interest is in corneal transplant,” she said. “The technology has advanced to the point where we can transplant just a thin layer of membrane to be successful, and it is exciting to be in the forefront of that,” Dr. Sundararajan said. “Medical cornea allows us to look at several conditions, including corneal ulcers; there is also overlap with uveitis and scarring disorders, and the multidisciplinary aspects are very compelling to me. The UW is uniquely positioned in cornea and uveitis with our large catchment area.”
In her research, Dr. Sundararajan has worked closely with Dr. Russell Van Gelder, MD, PhD, Bucey Professor and Chair, using his work in genetic sequencing of pathogens and applying that to corneal ulcers. This work aims to identify a pathogen from the corneal ulcer in a matter of hours and to choose the proper medication.
Last fall Dr. Sundararajan and her husband, Abhishek, welcomed a daughter, Ayanta. She enjoys reading and exploring the outdoors in her spare time.

Philanthropy: Celebrating the Bishop Foundation and 40 years of vision science research
After building a career in lumber, roofing, and banking in the Pacific Northwest, Edward Bishop and his wife, Lillian, established the Bishop Foundation in 1962 to advance eye research. The foundation set forth a bold purpose: “the cure of diseases of the eye, the correction of faulty vision, [and] the relief of needy sufferers from eye afflictions.” Mr. and Mrs. Bishop wished to support scientists working on the big unanswered questions in vision science.
In 1975, the foundation became interested in research conducted at UW Medicine and the Department of Ophthalmology. According to Emeritus Professor Robert Kalina, MD, the Bishop Foundation established the first professorship in the department’s history. Professorships help to recruit and retain talented scientists, bestow the holder with recognition, and provide a reliable source of funding for lab research.
"The Bishop Professorship added a foundation for discovery in our department that led to more named positions over many years and continues to this day, " Dr. Kalina said.
Robert Rodieck, PhD, held the Bishop Professorship from 1978 to 1997 and was known for significant contributions to visual neuroscience. Kris Palczewski, PhD held the Bishop Professorship from 1999 to 2005. Palczewski’s laboratory is best known for solving the structures of different forms of rhodopsin.
Jay Neitz, PhD, has held the Bishop Professorship since 2009. Jay and his collaborator (and spouse) Grace Hill Chair Maureen Neitz collaborate in their studies of the visual system. Their laboratories focus on developing gene therapy for cone-based vision disorders; investigating the role of genetic variability in cone photopigments in eye diseases such as macular degeneration, myopia, and glaucoma; and understanding the physiological basis for color perception. They have also mentored dozens of graduate students and postdoctoral researchers.
According to Dr. Neitz, the professorship has made a huge difference in the work the Neitz laboratories have accomplished. It has allowed their group to explore exciting new areas of research, and they have made groundbreaking discoveries in vision science that would not have been possible without the Bishop Foundation’s support.
We extend deep gratitude to the Bishop Foundation for their partnership in investing in vision science over 40 years.
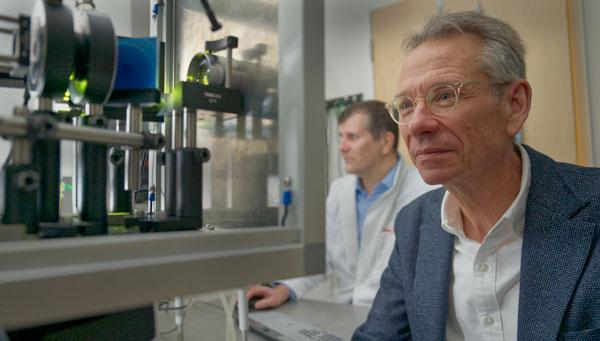
Education: 49th annual Resident Alumni Day and graduation
The 49th annual Department of Ophthalmology Resident Alumni Day was held June 17, 2023, in the Orin Smith Auditorium at UW Medicine South Lake Union.
The keynote speaker was Kuldev Singh, MD, MPH, Professor of Ophthalmology at Stanford University, speaking on “Glaucoma Innovation and the Looming Public Health Crisis.”
Four graduating residents and four graduating fellows presented their research projects to the audience.
At the graduation ceremony held in the evening, Hannah Hashimi, MD, now a fourth-year resident, received the Resident Research Award for her presentation on “Effects of Social Determinants of Health on Preferred Practice Patterns in Glaucoma.” Andrew Chen, MD, Assistant Professor, was honored as the full-time Teacher of the Year.
The graduation event honored fellows Matt McKay, MD; Alexandra Van Brummen, MD; Erin Godbout, MD: Kareem Sioufi, MD and Gabrielle Turski, MD. Dr. McKay is joining the faculty of Harvard Medical School and the Massachusetts Eye and Ear Infirmary, while Drs. Godbout and Sioufi are headed to private practice in oculoplastics and medical retina, respectively. Dr. Van Brummen is staying at UW to complete a second fellowship in oculoplastics, and Dr. Turski is moving to the University of Virginia to complete an additional fellowship in vitreoretinal surgery. Graduating residents Alex Legocki, MD (oculoplastics fellowship); Preston Luong, MD (private practice comprehensive); Connor Nathe, MD (private practice comprehensive); Grace Su, MD (cornea fellowship); and Philina Yee, MD (glaucoma fellowship) were also honored.




InSight Newsletter Spring 2023
UW Department of Ophthalmology
InSight Newsletter | Spring 2023
Welcome to InSight
Welcome to the Spring 2023 edition of the Department of Ophthalmology InSight Newsletter
Spring is a beautiful time in Seattle and especially at the University of Washington, with the cherry blossoms in bloom on the Quad. With the renewal of the season, we are pleased to present our new edition of the InSight newsletter.
The research spotlight in this issue shines on Associate Professor Kathryn Pepple, MD, PhD, who recently received a three-year grant from the Foundation Fighting Blindness to study treatments for uveitis resulting from gene therapy. Dr. Pepple’s lab is at the forefront of understanding how immune mechanisms cause ocular inflammatory disease. This highly competitive award will allow her lab to understand how we can potentially minimize this unwanted complication of gene therapy in the eye.
In our patient care feature, you will learn about the work of one of our newest faculty members, Clinical Associate Professor Eugene May, MD, who has established a neuro-ophthalmology clinic within the MS Center on the UW Medical Center-Northwest campus, dedicated to addressing the visual issues that individuals with multiple sclerosis face.
The Dawn’s Light Foundation, created by Chris and Jenny Carlson, is supporting important work - the diagnosis and management of inherited retinal diseases, including a generous gift to sponsor a one-day conference last fall.
Finally, in our education spotlight, meet the incoming ophthalmology residents joining us in July 2023. Our education team, led by Residency Program Director and Robert E. Kalina Professor Parisa Taravati, MD completed the Herculean annual task of reviewing over 600 applications for our five residency positions and interviewing dozens of candidates for our program. We are fortunate once again to have matched well within our top 5% of candidates, a testament to the competitiveness of our program nationally.
We hope you enjoy our spring update!
Russell Van Gelder, MD, PhD, Professor and Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Research Spotlight:
Grant to study prevention of uveitis in ocular gene therapy
Associate Professor Kathryn Pepple, MD, PhD, has received a three-year grant from the Foundation Fighting Blindness to study ocular gene therapy associated with uveitis and test prevention strategies.
“Gene therapy is an amazing technology for patients with inherited eye diseases,” Dr. Pepple said. “With gene therapy, we can hope to restore sight and to prevent blindness in a way never possible before. Inflammation in the eye following gene therapy administration, or gene therapy-associated uveitis, has been identified in several clinical trials. This inflammation is a potential barrier to gene therapy for all patients.”
Dr. Pepple said the goal is to identify a safe and effective treatment strategy to prevent gene therapy-associated inflammation for all patients.
“Any approach we can develop that improves therapeutic delivery and patient outcomes will be beneficial. Looking at inflammation not as a barrier to this great technology but as something that everybody is dealing with, and planning for it, will help make gene therapy an even better treatment in the long run.”
To understand why gene therapies delivered by AAV vectors cause uveitis, Dr. Pepple will collaborate with Glenn Yiu, MD, PhD at UC Davis, to study the problem in mice and non-human primates. They will also test a novel gene therapy vector designed to block innate immune responses in combination with medications used to treat uveitis to identify an effective strategy for human gene therapy patients.
For the past 10 years, Dr. Pepple’s lab at South Lake Union has studied uveitis in rodent models of disease. Dr. Pepple and her team have identified specific cytokines — small proteins crucial to our immune system response — involved in different stages of eye inflammation. This work was recently published in Experimental Eye Research PMID: 35921962. Using animal models, her lab has also tested novel anti-inflammatory therapies in collaboration with industry partners. A recent collaboration involved a Seattle biotech company that has developed a new molecule for blocking T-cell activation. T cells are immune cells responsible for initiating many forms of autoimmune uveitis. This work was published in the March edition of Translational Vision Science and Technology (PMID: 36976157).
Dr. Pepple’s research and clinical efforts all address her central career goal to prevent blindness in her patients with uveitis through effective medical management of ocular inflammation. She recently gave a talk to the Department of Ophthalmology Community Action Board about her work.
“Even though many medications are available for patients with uveitis, treatment failures, and side effects can leave some patients without good disease control. New and better therapies are still needed. Using our animal models of uveitis, we have identified immune cells and cytokines that are important in driving chronic inflammation in the eye. The next step is to confirm this data using human tissue samples.”
To achieve this new goal, Dr. Pepple will collect patient samples to form the University of Washington Ocular Inflammation Biospecimen Repository. She explained that the biorepository would provide critical confirmation about the inflammatory signaling molecules and pathways active in human eyes with uveitis.
“Furthermore, based on our data in mice, we predict we will identify distinct cytokine profiles in eyes with different types and stages of uveitis. Ultimately, we hope to use this molecular information to better tailor treatment strategies for our patients with uveitis.”
Dr. Pepple’s research has been supported by grants from the National Institutes of Health, Foundation Fighting Blindness, Research to Prevent Blindness, and generous gifts from donors, including Graham and Brenda Siddall and Mark J. Daily, MD

Patient Care Spotlight:
Meet Neuro-Ophthalmologist Dr. Eugene May
With the support of the Department of Ophthalmology and the UW Multiple Sclerosis Center, Clinical Associate Professor Eugene May, MD has established a neuro-ophthalmology clinic within the MS Center on the UW Medical Center-Northwest campus, dedicated to addressing the visual issues that individuals with multiple sclerosis face.
“I see patients once a week in the MS clinic at Northwest,” Dr. May said. “It is unusual to have immediate access to a neuro-ophthalmologist on-site in an MS clinic. We can also use optical coherence tomography to monitor patients and teach the MS fellow.”
Dr. May is nationally recognized for his expertise in multiple sclerosis and has recently served as a National MS Society board member.
“There has been remarkable progress in treating MS during my career,” he said. “There are now 19 FDA-approved medications for MS treatment, and we have a far better understanding of MS than when I started.”
Dr. May joined the full-time neuro-ophthalmology faculty of the UW Department of Ophthalmology in April 2022, with appointments in ophthalmology and neurology. He sees patients at the UW Medicine Eye Institute at Harborview, Harborview 4-West Clinic, and the VA Puget Sound Health Care System.
Dr. May was born and raised in New Orleans and received a Bachelor of Science in Engineering from Tulane University.
“I thought I would be a pediatrician until I took a neurobiology course in college, so I went into neurology. In my first year of medical school, I began the path to neuro-ophthalmology,” he said. “What I find interesting about neuro-ophthalmology is that most cases are difficult and have many possible causes, and it's up to us to figure out what is wrong and the best treatment.”
He received a US Army Health Professions Medical Scholarship to the University of Chicago Pritzker School of Medicine, where he became interested in the brainstem neuroanatomy of the eye-movement control system. Dr. May completed a neurology residency and a neuro-ophthalmology fellowship at Walter Reed Army Medical Center in Washington, DC. He was assigned to the ophthalmology and neurology training programs at Madigan Army Medical Center, where he was on the faculty for five years.
Between 1997 and 2022, Dr. May was on the medical staff of the Swedish Medical Center in Seattle and a neuro-ophthalmologist at the Swedish Neuroscience Institute. He was a longtime clinical faculty member, volunteering to teach ophthalmology and neurology residents, as well as seeing patients in the 4West clinic with the residents.
Dr. May and his wife, Patti, an obstetrician at Swedish in Issaquah, have an adult son and daughter. They enjoy spending time outdoors and have hiked worldwide, including climbing Mount Kilimanjaro several years ago.

Philanthropy Spotlight: Dawn's Light Foundation supports research into inherited retinal diseases
When Chris and Jenny Carlson’s son couldn’t see the NEO-WYSE comet, it began a journey for the family that resulted in the creation of the Dawn’s Light Foundation, which supports research into Inherited Retinal Diseases (IRDs).
Through genetic testing, their son Lucas was diagnosed with retinitis pigmentosa. Often diagnosed in childhood or adolescence, retinitis pigmentosa (RP) is an inherited retinal disease, causing progressive loss of night and peripheral vision. The condition often leads to legal blindness and sometimes complete blindness.
Jenny and Chris, who recently retired from the Fred Hutchinson Cancer Center after a career as a genetic epidemiologist, set about creating a foundation to support research into IRDs.
“Ironically, I spent my career studying the genetics of human disease at the Hutch, and then suddenly we found ourselves in genetic counseling as an affected family,” Chris Carlson said. “But we are inspired to use our resources to push things forward. Creating new therapies to treat these diseases will take time and investment.”
In September 2022, sponsored by a generous gift from the Dawn’s Light Foundation, the UW Department of Ophthalmology held a Vision Insights conference at UW Medicine South Lake Union, discussing the diagnosis and management of IRDs.
UW Department of Ophthalmology faculty Associate Professor and Vice Chair for Research Jennifer Chao, MD, PhD and Assistant Professor Debarshi Mustafi, MD, PhD led a featured panel of clinicians, researchers, and patient speakers to discuss current practices and the future of IRD treatment.
The Chao laboratory is working to create models of retinal degenerative diseases that can be used to discover potentially therapeutic drugs. The laboratory takes blood samples from volunteers affected by retinal degenerative diseases to create patient-specific stem cells and grow them into retinal cells to study.
“Ultimately, our group is focused on discovering new drug therapeutics that could benefit those affected by inherited retinal degeneration,” Dr. Chao said.
The Mustafi laboratory is applying sequencing technology to more accurately reveal pathogenic variants that lead to IRDs, especially in the pediatric population.
“Using isolated blood samples from affected IRD patients and their families, our lab can carry out genome sequencing to identify novel pathogenic variants of disease and reconstruct disease haplotypes, which has implications for interpreting disease risks in IRDs for patients and their families,” Dr. Mustafi said.
At the Vision Insights conference, Dr. Mustafi discussed pediatric diseases and new emerging genetic sequencing technologies that have the potential to provide a faster and more accurate diagnosis. They were joined by Research Associate Professor Ram Sabesan, PhD, who studies high-resolution functional imaging of the retina in IRD patients, and Timothy Cherry, MD, Assistant Professor and Principal Investigator at the Seattle Children’s Research Institute, who highlighted how his lab is using model systems called retinal organoids to study IRDs. The event also included a patient and family panel.
“It was a very successful event in that it rallied the community of patients, researchers, and clinicians around the study of IRDs,” Carlson said. “We hope that it can happen again in the future.”

Education Spotlight:
Welcome to our Ophthalmology residents in the class of 2027
We are excited to announce the incoming residents joining us in July 2023. Their first year is a joint internship with the Department of Internal Medicine. Learn more about our residency program at ophthalmology.washington.edu/education/residency
They are:
Dany Hage, Tulane University
Johnson Huang, University of Washington
Deborah Im, University of Southern California
Jonathan Le, University of Wisconsin
Marcus Turner, University of California, San Francisco

2022 Community Report now available
InSight, the 2022 Community Report of the Department of Ophthalmology, has been published and is available online HERE.
Because of the COVID-19 pandemic, this is the first Community Report in three years. Despite the significant challenges during this time, we have continued to pursue our singular mission: to alleviate suffering from eye disease. We continue to do this through our robust research programs, outstanding patient care, educational programs to train the next generation of physicians, and by gifts from generous donors and grateful patients. We have had a remarkable year in the department in each of these areas and are delighted to share our progress with you.
InSight Newsletter Winter 2023
Message from the Chair
2023 is in full swing, and we are pleased to present our Winter edition of the InSight newsletter.
The research spotlight in this issue shines on Assistant Professor Debarshi Mustafi, MD, Ph.D., and Associate Professor Andrew Stacey, MD, highlighting their collaborative efforts to develop genetic testing to confirm a diagnosis of retinoblastoma in neonatal patients. They were awarded a three-year grant from the Gerber Foundation to implement this technology in clinical practice.
We are pleased to introduce our newest faculty member, Assistant Professor Eric Duerr, MD! Dr. Duerr joined us last fall as a comprehensive ophthalmologist at the Eye Institute at Harborview. Learn more about his passion for patient care and academic medicine.
The Karalis Johnson Retina Center at South Lake Union celebrated four years last month. The Center continues to build on donor Angie Karalis Johnson’s vision to create a center where patients can find the finest care available anywhere and participate in research designed to preserve and restore vision lost to retinal disease.
Finally, in our education spotlight, meet the incoming fellows joining us in July 2023, and learn where some of our current fourth-year residents will continue their graduate medical education.
We hope you enjoy our winter update!
Russell Van Gelder, MD, Ph.D., Professor and Boyd K. Bucey Chair, UW Medicine Department of Ophthalmology
Research:
Rapid neonatal diagnosis of retinoblastoma awarded a grant by the Gerber Foundation
Drs. Debarshi Mustafi and Andrew Stacey, saw an opportunity to merge their research and clinical interests after a discussion in the operating room examining retinoblastoma patients at Seattle Children’s Hospital.
Retinoblastoma is a devastating eye cancer that affects about one in 100,000 children. In past times, the mortality rate for this cancer was high, and survivors often lost their eyes to the disease. Retinoblastoma comes in two varieties – inherited and sporadic. While in some cases, a family history will suggest genetic disease, in cases where there is no family history, it is important to determine if the child carries the genetic risk factor in their whole body or just in the affected eye. In the former case, the other eye must be examined under anesthesia frequently, while in sporadic cases, the fellow eye is very unlikely to be affected. The current timeline to obtain genetic testing to confirm a diagnosis of genetic retinoblastoma took weeks to months and necessitated repeated exams under anesthesia for these neonatal patients while the results were pending. A more rapid genetic test result would not only alleviate this but would alter treatment decisions, such as initiating chemotherapy treatments carrying some risk and sometimes deciding whether a cancerous eye needs to be removed.
Drs. Mustafi and Stacey set out to find a solution to this pressing problem. They utilized an emerging technology being developed in the Mustafi and Van Gelder laboratories, termed adaptive sequencing, which allows one to selectively sequence specific segments of the genome to target the retinoblastoma gene. They demonstrated that after the isolation of DNA from the blood from a patient, they could deliver a definitive diagnosis of genetic retinoblastoma in a matter of days. Drs. Mustafi and Stacey recently published their work in Ophthalmic Genetics and were awarded a three-year grant from the Gerber Foundation to implement this technology in clinical practice.
Patient Care:
Meet Eric Duerr, MD: A Talented Physician with a Passion for Teaching
Eric Duerr, MD, assistant professor of ophthalmology and comprehensive ophthalmologist, grew up in Pittsburgh, where he developed a love for basketball while playing on his high school team. His father, a gastroenterologist, was a significant influence on his decision to pursue a career in medicine. Dr. Duerr was recruited to play center on Case Western University’s basketball team, where he competed against some of the best teams in the Division III University Athletic Association conference.
Despite his success on the court, Dr. Duerr's true passion was always in medicine. He studied biology at Case Western and attended medical school at the University of Pittsburgh. There, he met his future wife, Stephanie Chen, MD, who had previously worked as an ophthalmology technician. Today, Dr. Chen is a neurosurgeon and fellow at the University of Washington Department of Neurosurgery.
Dr. Duerr completed his residency and fellowship in glaucoma at Bascom Palmer Eye Institute in Miami, Florida. He chose academic medicine because he loves serving patients and wants to positively impact the next generation of physicians.
“I truly enjoy working with the residents in our program,” he said. “I believe I learn a great deal from these young doctors.”
We are thrilled to have Dr. Duerr join our team and look forward to seeing the positive impact he will make on our patients and residents in the coming years.
Philanthropy:
Karalis Johnson Retina Center marks four years
January marked the fourth anniversary of the opening of the Roger and Angie Karalis Johnson Retina Center. This state-of-the-art clinical and research facility at South Lake Union brings together our outstanding UW retina and uveitis clinicians, the most up-to-date equipment, and our cutting-edge research teams.
The Center fulfilled a long-standing dream of donor Angie Karalis Johnson. Angie, who worked for decades with her late husband, ophthalmologist, and emeritus clinical faculty member Roger Johnson, MD, saw first-hand the terrible impact of blinding retinal disease on patients. The goal of the Center is to create one location where patients can find the finest patient care and participate in research designed to improve outcomes in the future.
Angie and Roger had previously endowed the Roger Johnson Lectureship at Seattle Children’s, which brings top pediatric ophthalmologists to lecture in Seattle. Years later, they endowed the Roger H. Johnson Award for Macular Degeneration. This prize is given to the scientist or clinician who has significantly contributed to the understanding or treatment of age-related macular degeneration.
Macular degeneration is a debilitating condition that affects the macula, a region in the retina responsible for sharp, central vision. People who suffer from it often lose their central vision. According to the National Eye Institute, more than 5.44 million people in the U.S. are projected to have vision loss from age-related macular degeneration by 2050.
“Angie’s gift has been transformative over the last four years,” says Russell Van Gelder, MD, Ph.D., Professor and Boyd K. Bucey Chair. “Thanks to her generosity, we have one of the nation’s most outstanding facilities to care for patients with macular degeneration and other retinal diseases. The center is equipped with state-of-the-art research equipment and staffed by the nation’s best researchers. I anticipate many advances — helping millions of people — will flow from Angie’s remarkable gift.”
Education
We are excited to announce the incoming fellows joining us in July 2023.
Pediatric Ophthalmology: Jeannette Stallworth is currently completing her ophthalmology residency at the University of California San Francisco.
Oculoplastics: Alexa Van Brummen completed her ophthalmology residency here at the University of Washington and is currently completing a fellowship in pediatric ophthalmology at UW/Seattle Children’s Hospital.
Vitreoretinal Surgery: Nathan Agi is currently completing his ophthalmology residency at NJMS Rutgers Department of Ophthalmology and Visual Sciences.
Uveitis: Yamini Attiku completed her ophthalmology residency at All India Institute of Medical Sciences and is currently completing a Medical Retina fellowship at Bascom Palmer Eye Institute in Miami, Fla.
We are also excited to share fellowship match results for our UW fourth-year residents graduating this summer.
Alex Legocki will pursue an Oculoplastics Fellowship at Allure Laser Center & Medispa in Seattle.
Grace Su will be pursuing a Cornea Fellowship at UC Irvine.
Philina Yee will be pursuing a Glaucoma Fellowship at UC Irvine.
InSight Newsletter Fall 2022
InSight Newsletter | Fall 2022
Welcome to InSight
Message from the Chair
Welcome to the Fall 2022 edition of the Department of Ophthalmology InSight Newsletter.
Fall is upon us, and we are pleased to present our latest edition of the InSight newsletter.
The research spotlight this issue shines on Dan and Irene Hunter Associate Professor of Ophthalmology Aaron Lee and Klorfine Family Chair and Associate Professor Cecilia Lee, jointly awarded a $33 million, four-year grant as part of the Bridge to Artificial Intelligence (Bridge2AI) program, a new initiative by the National Institutes of Health to expand the use of artificial intelligence in biomedical and behavioral research. It is the largest grant award in department history. Artificial intelligence holds great promise for enabling research breakthroughs and improving clinical care; you can read more about this transformative project in the accompanying article.
Glaucoma remains the second leading cause of vision loss in the United States. Our patient care spotlight is on our glaucoma service, which is central to ourmission of eliminating suffering fromeye disease. We are pleased to welcome back Dr. Karine Bojikian to the department this year as Assistant Professor. Karine completed her ophthalmology residency at UW in 2020 and was previously a visiting scientist here. Her expertise includes the surgical and medical management of standard and complex glaucoma and cataract cases, including laser treatment and minimally invasive glaucoma surgery. Her research focus investigations encompass optical coherence tomography angiography applications in the diagnosis and disease progression monitoring of glaucoma.
Thanks to our generous donors, we are honored to announce that Dr. Ruikang (Ricky) Wang, Ph.D., was recently appointed to the George and Martina Kren Endowed Chair in Ophthalmology Research. Dr. Jennifer Chao, MD, Ph.D., Vice Chair for Research, was recently appointed to the Gordon and Joan Bergy Endowed Professorship in Ophthalmology. Learn more about their appointments and the donors in this issue.
Finally, in our education spotlight, you will learn more about the unique collaboration between the residency programs at Madigan Army Medical Center and UW. Our PGY-4 Ophthalmology residents each spend part of their rotation at Madigan at Joint Base Lewis-McChord, where they have the opportunity to perform refractive surgery for active-duty service members. In exchange, two Madigan residents each spend a month at UW for an ophthalmology trauma rotation. It is truly a win-win partnership for both programs.
Russell Van Gelder, MD, PhD, Professor and Boyd K. Bucey Chair
Research Spotlight: Strengthening the power of artificial intelligence through intentional data collection
Cecilia Lee, MD, MS and Aaron Lee, MD, MSCI (Lee Lab)
Associate Professors of Ophthalmology Aaron and Cecilia Lee have recently been awarded a $33 million, four-year grant as part of the Bridge to Artificial Intelligence (Bridge2AI) program, a new initiative by the National Institutes of Health to expand the use of artificial intelligence (AI) in biomedical and behavioral research. It is the largest grant award in department history.
AI holds great promise for enabling research breakthroughs and improving clinical care. The power of AI lies in its ability to analyze vast amounts of data and extract otherwise undetectable information, but this power is limited by the quality of the data used to develop AI models. Although exciting progress is being made in this field, the need for large, thoughtfully curated datasets remains a significant challenge.
The NIH Common Fund developed the Bridge to Artificial Intelligence (Bridge2AI) initiative to address this critical need. The Drs. Lee have been awarded one of the four Bridge2AI data generation grants for new biomedical and behavioral datasets designed for AI analysis.
“We will lead multisite efforts to create an ethically sourced, state-of-the-art dataset for type-2 diabetes mellitus (T2DM) research in this unprecedented project,” notes Dr. Cecilia Lee. “We will recruit 4,000 participants with diverse racial/ethnic backgrounds representing all stages of T2DM disease severity and collect complex multimodal data. This collaboration is structured with cross-disciplinary modules focusing on several interconnected aims, including team building, ethical oversight, training new AI researchers, and creating tools and standards for data collection. We hope that this dataset, while designed for T2DM, will also serve as a model for AI-based research into other diseases.”
The Lees’ computational ophthalmology lab has examined deep-learning models’ value in medical practice. In 2021, investigators tested seven algorithms designed to detect diabetic eye disease from retinal scans and found that just one met the performance of human screeners.
“These worked fairly well in the screening context. There didn’t seem to be any bias in detecting disease in people of different races, but there was a decrease in performance concerning people’s age. That is what this new project hopes to address,” Dr. Aaron Lee said. “If you don't have a well-constructed, balanced dataset, then the AI models will tend to fail in underrepresented groups.”
For more details about this project, read the UW Newsroom article here. To learn more about the Bridge2AI program, visit the Musings from the Mezzanine blog from the National Library of Medicine, watch this video about the Bridge2AI program, and read the NIH press release. Patient Care Spotlight: New Faculty Member Karine Bojikian, MD, Ph.D.
Glaucoma Service Overview
Glaucoma is the leading cause of irreversible blindness worldwide. The term ‘glaucoma’ describes a group of chronic eye conditions characterized by progressive damage to the optic nerve. The damage is often related to high intraocular pressures, but it can also happen at normal levels of intraocular pressure.
Glaucoma has no symptoms in its early stages. Half the people with glaucoma do not know they have it. Some people have no signs of damage but have higher than normal eye pressure (called ocular hypertension). These patients are considered "glaucoma suspects" and have a higher risk of eventually developing glaucoma.
“To lower the pressure, the most common treatment is prescription eye drops,” said Dr. Karine Duarte Bojikian, MD, Ph.D., who joined the Glaucoma division this past summer. “There are also laser and surgical treatments, with the same aim, to lower the eye pressure and prevent glaucomatous vision loss.”
A native of Sao Paulo, Brazil, Dr. Bojikian completed her first ophthalmology residency and glaucoma fellowship training at the Federal University of Sao Paulo. In 2011, Dr. Bojikian joined the UW as a visiting scientist, primarily in glaucoma research and published over 80 scientific works, including peer-review publications, book chapters, and abstracts in society meetings. She then completed her second ophthalmology residency training at the University of Washington in 2020. During her training here, she received several awards and distinctions for excellence in ophthalmology, including the Association of University Professors in Ophthalmology/Research to Prevent Blindness Research Award, the American Society of Cataract and Refractive Surgery Resident Excellence Award, and the National Eye Institute/ARVO Travel Grant Award. She completed a Heed Fellowship in glaucoma at the OHSU Casey Eye Institute & Devers Eye Institute in Portland, Oregon, in 2021.
Dr. Bojikian is a board-certified ophthalmologist specializing in glaucoma and cataracts. Her expertise includes the surgical and medical management of standard and complex glaucoma and cataract cases, including laser treatment and minimally invasive glaucoma surgery. Her research focus investigations encompass the applications of optical coherence tomography angiography in the diagnosis and disease progression monitoring of glaucoma.
“I am glad to be here at UW with the highest quality in medical and surgical care while supporting our patients through the journey of glaucoma care.’
Education Spotlight: Ophthalmology Resident Madigan Rotation
Resident rotation at Madigan and Harborview benefits both organizations
Our PGY-4 Ophthalmology residents each spend part of their senior year in a rotation at Madigan Army Medical Center at Joint Base Lewis-McChord, where they have the opportunity to work with Drs. Patrick Munson and Joshua Roe. Residents perform refractive surgery for active-duty service members during their time there with cutting-edge laser technology.
In exchange for our residents having the opportunity to work at Madigan, two Madigan residents each spend a month at UW for an ophthalmology trauma rotation. During the four-week rotation, the Madigan resident takes senior call at Harborview, where they can supervise the junior ophthalmology residents and participate in surgical emergencies, including ruptured globe operations.
Dr. Philina Yee, MD (PGY4), did her rotation at Madigan in August 2022.
“It was great learning how to use the femtosecond laser. I had never seen LASIK or PRK done before this rotation,” Yee said. “I loved my experience there, working with the population there of mostly younger people on active-duty service. We get to see the work at Madigan and appreciate those serving in the military and their families.”
Dr. Yee grew up in the Seattle area. After graduating from Cornell University with a BS in Neurobiology and Behavior and a minor in Global Health, she worked at the National Institutes of Health researching signal transduction in sensory neurons. She attended Case Western Reserve University School of Medicine, where her interest in ophthalmology blossomed. Dr. Yee was happy to return home to Seattle, where her family still resides, including her younger brother, a UW resident in internal medicine at Virginia Mason Medical Center.
Yee said her residency at UW Ophthalmology has been transformational.
“I think I have changed more as a person than any other time in my life during residency,” she said. “I have been involved in many complex cases and gained great experience; these four years have gone by so fast.”
Donor Spotlight
Faculty named to endowed positions thanks to generous gifts
Department of Ophthalmology faculty members Dr. Jennifer Chao and Dr. Ruikang (Ricky) Wang have recently been named to endowed appointments at the University of Washington.
“Congratulations to Dr. Chao and Dr. Wang! An appointment to an endowed professorship and endowed chair is one of our highest honors,” said Dr. Russell N. Van Gelder, MD, Ph.D., Professor and Chair of the Department of Ophthalmology. “We are grateful to these donors for their generous gifts to support continued excellence in patient care and research.”
Dr. Chao, MD, Ph.D., Vice Chair for Research, was recently appointed to the Gordon and Joan Bergy Endowed Professorship in Ophthalmology. Dr. Chao has been on the faculty at UW since 2009.
A retinal disease specialist, Dr. Chao has an active laboratory that studies retinal degenerative disorders. The Chao Lab is investigating potential applications of induced pluripotent stem cells (iPSCs) for treating eye diseases and identifying new drug therapies for eye diseases.
Inherited retinal degeneration is a significant cause of blindness. The Chao laboratory is working to create models of retinal degenerative diseases that can be used to discover potentially therapeutic drugs. The laboratory takes blood samples from volunteers to create patient-specific stem cells and grow them into retinal cells to study.
In support of the Department of Ophthalmology, in 2012, Joan Bergy provided funding for the Joan and Gordon Bergy Visiting Professorship series, which brings three outstanding vision scientists to visit and deliver scientific lectures each year. Several years ago, Joan moved to the Aljoya community on Mercer Island. She and Gordon had a beloved home in Hansville, Washington. After she made the difficult decision to sell the house, she decided to use the proceeds to fund an endowed professorship. Dr. Chao is Joan’s retina specialist at the Karalis Johnson Retina Center at South Lake Union.
“I am inspired by the visionary leadership of Dr. Van Gelder, who has led the UW Medicine Eye Institute and the Retina Center, and Dr. Jennifer Chao, whose ongoing research is the use of stem cells to restore patient vision,” Joan said. “What we do for ourselves dies with us, but what we give to others lives on,” she says. “And what could be more important than the gift of vision?”
A UW faculty member since 2011, Dr. Ruikang (Ricky) Wang, Ph.D., was recently appointed to the George and Martina Kren Endowed Chair in Ophthalmology Research. Wang is a professor with appointments in the Departments of Bioengineering and Ophthalmology at the UW and directs the Biophotonics and Imaging Laboratory.
The Wang lab is dedicated to developing biomedical imaging techniques for early diagnosis, treatment, and management of human diseases, especially retinal diseases.
His efforts have contributed to retinal findings in infants and adults with unprecedented precision, speed, and imaging resolution. Dr. Wang is widely credited with being the inventor of optical coherence tomography angiography (OCTA), a technique in which blood flow can be measured in all blood vessels in the eye non-invasively. This technique is now a standard testing modality in ophthalmology offices worldwide.
George Kren was born in Prague, Czech Republic, and emigrated to the U.S. in the early 1970s. In 1976 he co-founded Tencor Instruments, a company that later merged into KLA-Tencor. He was also instrumental in founding the Surfscan Division and acquiring the companies Censor in Lichtenstein and NanoPro in Germany. For many years he had a leading role in SEMI Standards, where he received the SEMI Lifetime Award in 2004. George is now retired and lives with his wife, Martina, in Monterey, California. George serves on the UW Medicine Eye Institute Community Action Board, and he and Martina are also helping to support an endowed professorship in advanced ocular imaging within the Department of Ophthalmology. Seattle/King County Eye Clinic
Miel Sundararajan, MD, and University of Washington Department of Ophthalmology Residents volunteer at annual eye screening event
Dr. Miel Sundararajan, MD, and Ophthalmology department residents volunteered at the Seattle/King County Eye Clinic held Oct. 20-23 at Seattle Center. The free community clinic offered vision screening, complete eye exams, reading and prescription eyeglasses to help those who struggle to access affordable eye care. Dr. Sundararajan serves as the director of outreach programs for the department