Retina implant shows promise in restoring vision
Research is making substantial progress in the use of retinal prostheses to restore vision in patients who are blind due to photoreceptor loss in degenerated retinas.
Retinal prostheses electronic devices that deliver electrical stimulation to the blind retina, inducing “artificial vision.” To date, three retinal prostheses have been approved for implantation outside of clinical trials, all of which are targeted at patients with retinitis pigmentosa.
UW Professor of Ophthalmology Lisa Olmos de Koo, MD, MBA, has been working on retinal prosthesis research for nearly 15 years, dating back to the original ‘Argus II’ device developed in Southern California. More recently, she has been working with an international team based at Stanford University developing the PRIMA prosthesis. She notes that a recent large clinical trial in Europe has yielded promising results for the device.
“Use of retinal prostheses has a strong upside,” Dr. Olmos said. “The large research pipeline offers hope for future advances in retinal prosthesis design and vision restoration for those blinded by photoreceptor loss. We are hoping to achieve vision restoration for those patients who don’t have any other options because of geographic atrophy.”
Geographic atrophy (GA) is an advanced form of dry macular degeneration characterized by the death (or atrophy) of cells in the central part of the retina, known as the macula.
“For many patients with GA, this is the only thing we can offer at present in terms of getting vision back,” Dr. Olmos said.
Dr. Olmos is collaborating with researchers at Stanford University and other institutions on the new device, which is designed to aid individuals blinded by dry age-related macular degeneration with geographic atrophy.
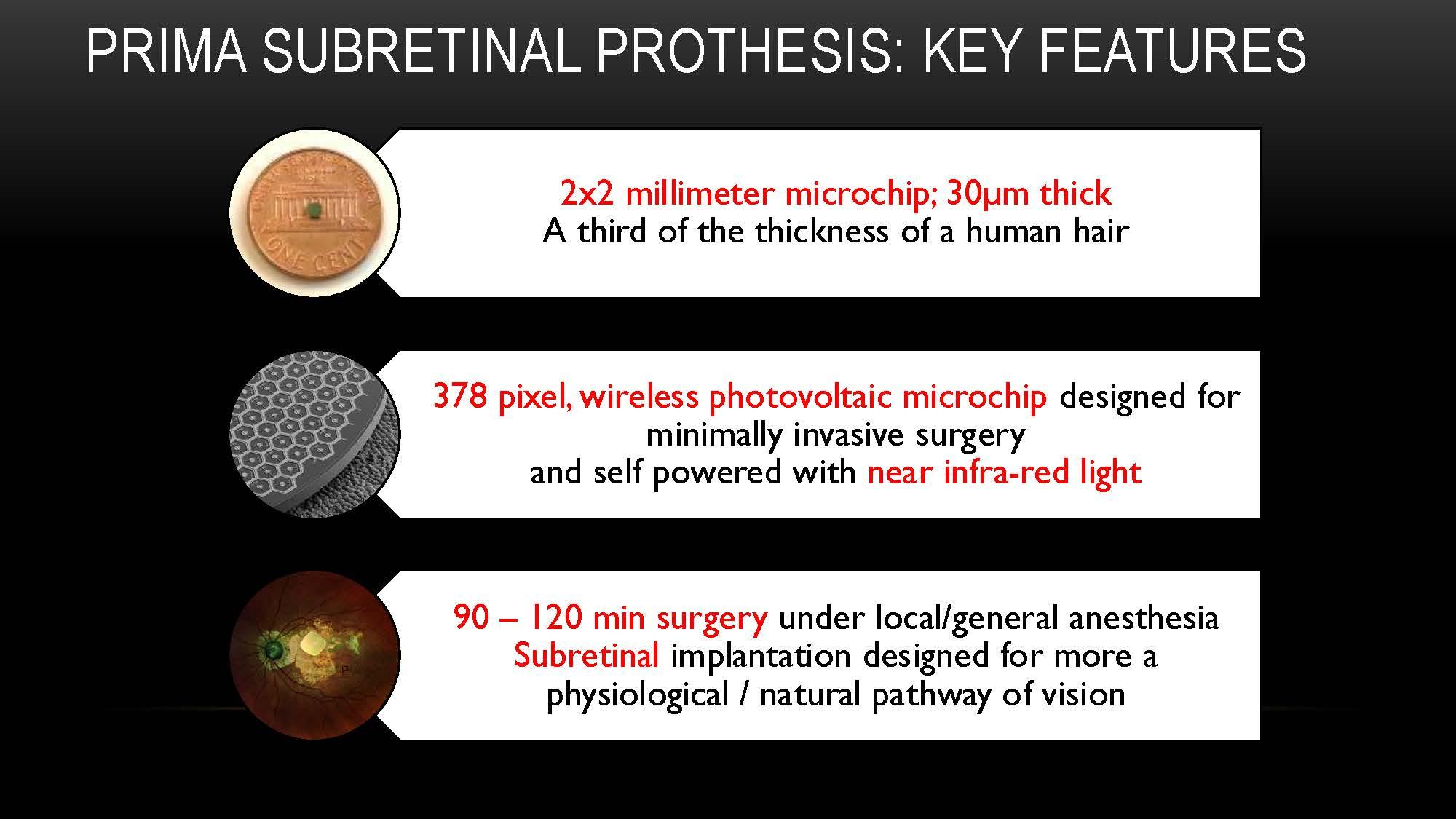
The PRIMA is a wireless, subretinal, photovoltaic microchip that is approximately one-third the thickness of a human hair and utilizes a near-infrared light source to power the implant. The nanoelectrodes stimulate remaining cells in the degenerated retina to induce visual phenomena. Once surgically implanted, the patient operates the device using a pocket-sized processor and wears specialized glasses equipped with a video camera. It is being developed by Science Corporation. The pivotal clinical trial of the device, known as the PRIMAvera study, involved 38 patients, primarily in Europe.
Patients in the clinical trials experienced significantly improved visual acuity with the PRIMA device.
PRIMA produces the best prosthetic visual acuity to date, Dr. Olmos said. Patients can use the device for reading letters, numbers, and words. Some patients can even read longer text. Dr. Olmos is a consultant to Science Corporation, which is developing the device and hopes to bring it to the U.S. market.